New Blood Test for IBS: Should You Seek It Out?
During a webcast on September 24, 2018, Mark Pimentel, MD of Cedars Sinai announced that a blood test for the diagnosis of diarrhea and mixed irritable bowel syndrome is now available based on the fact that IBS can start after food poisoning (PI-IBS).
This IBS test may be an interesting development for individuals who suffer from gastrointestinal (GI) symptoms, such as frequent diarrhea, gas and bloating, abdominal pain and distention, in terms of clarifying the cause of their issues. (Discount coupon for FODMAP Everyday® readers at end of article.)
However, the announcement of this test also raises a number of potential questions regarding who might benefit from this test. This article will explore these further.
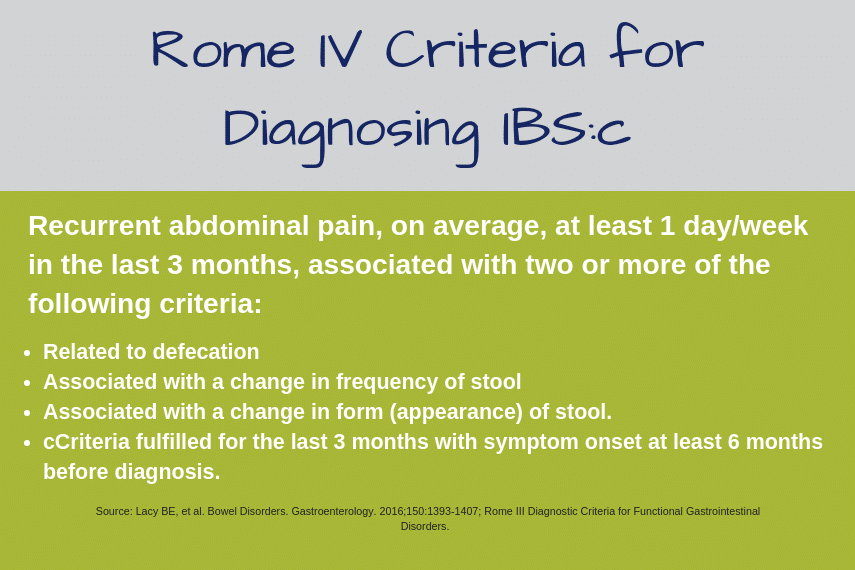
How is IBS Typically Diagnosed?
The ROME IV criteria for diagnosis of IBS were released by the ROME Foundation in 2016. The criteria include: recurrent abdominal pain on average at least 1 day per week during the past 3 months, that began more than 6 months previously, and meets 2 or more of the following: related to defecation, associated with a change in frequency or stool, and associated with a change in appearance of stool.[1]
The process can be complicated as many of these disorders have very similar or overlapping symptoms.
What is Post-Infectious IBS?
Post-infectious IBS (PI-IBS) is defined as IBS that results from a previous bacterial, viral or parasitic infection of the GI tract (sometimes called infectious gastroenteritis, or more simply, foodborne illness).[2]
It’s not yet known how exactly these pathogens lead to IBS, however researchers have suggested that these infections can lead to changes in the gut mucosa, gut motility and absorptive capacity of the gut.[3]
These reactions, individually or together, can cause significant changes to the GI tract and affect overall gut and immune function, as well as cause painful symptoms.
It’s important to note that not everyone who suffers from foodborne illness will develop IBS. A recent scientific review of prior studies calculated that on average, 1 in 9 people who experience infectious gastroenteritis will go on to develop IBS (or about 11%).[4]
In addition, post-infectious IBS is a small subset of the total IBS population, comprising about 6-17% of the total population of IBS sufferers[5].
Or put more simply, there’s many other factors besides foodborne illness that can be affect the development of IBS, including genetics, gender, age, ethnicity, physiological or psychological stress, childhood trauma and more[6] [7].
So where does the new ibs-smart™ test fit into all this? Read on.
How the Test Works
The blood test is based on two relatively large-scale studies (one study was published in 2015, the other has not yet been published) out of Dr. Pimentel’s Cedars Sinai lab.
The test can identify the presence of two antibodies, anti-CdtB and anti-vinculin, in blood samples. These antibodies are created in response to bacterial infection and have been found in individuals who have previously suffered from infectious gastroenteritis, thus serving as markers for PI-IBS.
Completing the test requires a simple blood sample, which then generates a result of “positive” for IBS (see “About the Test” below for more details).
Accuracy of the Test
While a previous version of the test was fairly accurate, Dr. Pimentel reports that this new version of the test brings an improved level of accuracy.
If someone receives a positive test result, they can assume with more than 90% confidence that they have IBS. However, the test has a fairly low detection rate (or “sensitivity” in scientific terms) and may miss up to 50% of IBS cases (e.g. you may get an “inconclusive” result and actually have IBS), so there are important tradeoffs to consider.
Potential Benefits of a Blood Test to Aid Diagnose of IBS
Worldwide, approximately 12% of the world’s population has IBS, and these patients account for more than 50% of consultations with gastroenterologists globally. [8] [9]
The idea of a rapid blood test to diagnose IBS is very attractive for many patients who often spend years in physical and financial suffering, living with uncomfortable and unexplained GI symptoms, and undergoing dozens of costly or invasive clinical tests before receiving a diagnosis.
A test that could shortcut this process would provide peace of mind and improved quality of life, not to mention significant time and cost savings for patients and healthcare practitioners alike. Dr. Pimentel affirms these aspirations – “We are trying to stop the madness of these patients running around getting test after test.”
From the dietitian’s perspective, Andrea Hardy, RD, of Ignite Nutrition, believes this new blood test has the potential to improve the confidence of diagnosis for individuals with post-infectious IBS. Hardy, a Canadian dietitian who specializes in gut disorders, notes, “Where I often see gaps in diagnosis has to do with the physician’s confidence in diagnosing IBS, and the understanding IBS is a real condition and not merely a diagnosis of exclusion. I feel this test may serve to validate and improve understanding around IBS.”
The test can also help individuals manage their IBS in some cases. As Dr. Pimentel notes, “If you have IBS and you’re positive on the test, it means it came from food poisoning. Therefore, you know if you get food poisoning again, you’re more susceptible to getting these anti-bodies and making your IBS worse.”
This knowledge can help steer patients toward being more careful with food selection in terms of avoiding risky scenarios where bacteria and pathogens may be present.
Potential Drawbacks to the New IBS Blood Test
While this new blood test has the potential to rapidly identify PI-IBS, the science remains unclear how definitive these results will be when tested in larger or more diverse populations than the two initial studies.
Additionally, the test is not able to diagnose IBS that results from other risk factors or causes beyond foodborne illness, and it is not appropriate for individuals who suspect IBS-C (constipation predominant IBS), as this form of IBS has a different presentation and does not correspond to the anti-vinculin and anti-CdtB markers.
This suggests that the test may not be a reliable substitute for the standard, and highly validated, clinical diagnostic process for IBS.
It’s also important to note that many individuals suffer from multiple gastrointestinal disorders or a combination of gut issues and autoimmune diseases, such as celiac disease, IBD (Crohn’s disease or ulcerative colitis), food allergies or chemical intolerances.
Because the new IBS blood test provides a single diagnostic indicator, without other tests being conducted, more serious issues may go unexplained or untreated; leading to long-term health problems or serious complications.
Dr. Pimentel agrees, “I would not use this test on the “amazing enigma” or very challenging patient who presents with myriad symptoms or complications.” The ideal candidate for this test? “The person who has diarrhea or mixed IBS, bloating gas and distention, but no red flags, no blood in the stool, no weight loss. That is the patient who would possibly benefit from the test.”
Hardy also concurs, “Because the test is only validated in those with post-infectious IBS, a lot of care and attention will need to be given as to the appropriate use of this test.”
Hardy sees the test as a potential tool for patients who may not be good candidates for other types of invasive testing or who may have a long wait to see their gastroenterologist, as well as those patients who do not present with red flags for other gut disorders and are seeking additional clarity around their IBS diagnosis in the form of a blood test confirmation.
The Bottom Line
The ibs-smart™ blood test offers the promise of a new tool in the physician’s arsenal for diagnosing IBS and may serve to reduce time to diagnosis for patients with a specific type of IBS that occurs following acute infection.
This can improve patient quality of life, decrease patient medical costs and reduce the economic burden on the healthcare system. However, the test should not be used as the sole diagnostic tool for IBS due to a number of important limitations.
What Else Is New?
To read about some other new approaches to the detection and treatment of IBS read Success Team Member, Erica Ilton, RDN two-part series about her experience at the 2018 scientific meeting of the American College of Gastroenterology (ACG). You can find the first article Is It Time To Rename Functional Gastrointestinal Disorders? here. And the second article New Use for the Low FODMAP Diet, a Test for IBS, and Gluten in Restaurant Food here.
About the Test
Who should consider the test: Individuals who have unexplained diarrhea, gas, bloating and/or abdominal distention. Note: individuals should always rule out celiac disease with proper testing before or alongside an IBS diagnosis.[1]
How to get the test: The test kit is available by talking to your doctor or gastroenterologist and/or you can order it online via the ibs-smart™ website (www.ibssmart.com).
What is required: A simple blood test, which can be collected at your local doctor’s office or medical laboratory. Results from the test will be sent directly to your physician.
Cost: The test kit costs $220. This does not include the costs of a blood draw, nor a doctor’s visit to discuss your results. Your insurance may cover some, all or none of the costs, depending on your individual level of coverage. See the 25% discount coupon below for FODMAP Everyday® readers.
Before you test: Talk with your doctor or gastroenterologist or primary care physician to see if this test might be appropriate for you. The test can only identify IBS that has arisen due to previous food poisoning/foodborne illness. It cannot diagnose IBS that may arise from other factors nor can it diagnose IBS-C.
[1] Irritable bowel syndrome in adults: diagnosis and management | Guidance and guidelines | NICE. (2018). Retrieved from https://www.nice.org.uk/guidance/cg61/chapter/1-Recommendations#diagnosis-of-ibs
REFERENCES
[1] Lacy BE, Patel NK. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017;6(11):99. Published 2017 Oct 26. doi:10.3390/jcm6110099
[2] IBS, U., & Us, C. (2018). Post-infectious IBS. Retrieved from https://www.aboutibs.org/what-is-ibs-sidenav/post-infectious-ibs.html
[3] Beatty JK, Bhargava A, Buret AG. Post-infectious irritable bowel syndrome: mechanistic insights into chronic disturbances following enteric infection. World J Gastroenterol. 2014;20(14):3976-85.
[4] IBID.
[5] Are There Risk Factors for Developing IBS?. (2018). Retrieved from https://www.healio.com/gastroenterology/curbside-consultation/%7Bf6c033b4-4bcc-4b2e-aaee-a357991f4560%7D/are-there-risk-factors-f
[6] IBID.
[7] Irritable bowel syndrome: Novel views on the epidemiology and potential risk factors
Rey, E. et al. Digestive and Liver Disease, Volume 41 , Issue 11 , 772 – 780
[8] Lacy BE, Patel NK. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017;6(11):99. Published 2017 Oct 26. doi:10.3390/jcm6110099
[9] Corsetti M, Whorwell P. The global impact of IBS: time to think about IBS-specific models of care?. Therap Adv Gastroenterol. 2017;10(9):727-736.








People who live in New York state cannot get this blood test to do the kit. New YOrk has a rule that they dont ship blood out of state? What to do since traveling is not a current option francine
Thank you for the update, which we were not aware of, but is not surprising. Things are up-in-the-air in regard to so many different things. I would contact the company and discuss this with them. We certainly cannot provide any answers that would be more accurate than their advice.