The Keto Diet and IBS
There is a lot of buzz about the ketogenic diet in the media these days in relation to weight loss, athletic performance and even irritable bowel syndrome (IBS). You may have heard about keto and wanted to see what it’s all about.
This article will describe the diet – both the original classic, ketogenic diet and the “modern-day ketogenic diet” – and outline a number of pros and cons in relation to weight loss and managing symptoms of IBS.
What Is The Ketogenic Diet?
The classic ketogenic diet (CKD), in its truest form, has been around for more than a century. It was originally used in the early 1900s as a treatment for intractable epilepsy, or epilepsy in children that was resistant to the effects of multiple medications.
The diet experienced a resurgence in pediatric neurological units in the US in the late-1980s and continues to be used by physicians and registered dietitians to control seizures.
The brain and most of our body’s systems naturally utilize carbohydrates as their preferred fuel, because they are a source of quick energy. Carbohydrates break down rapidly into glucose, which can be used by cells throughout the body or stored for later use in the liver and muscles.
Dietary fat and protein are slower to be broken down by our gastrointestinal (GI) tract and transported to our cells. When the body does not have sufficient stores of glucose, it breaks down dietary fat (fat you eat) or stored fat (fat from fat cells) producing ketone bodies, which are then used to fuel the body and brain. This ketone production response to low glucose levels is designed to protect our biological systems from shutting down due to lack of fuel and is often called the “starvation response.”
Production of ketone bodies is where the “keto” part of the ketogenic diet comes in. For reasons that scientists are still a bit baffled by (though many strong theories exist), high levels of ketones seem to have positive effects on neurological regulation. Besides epilepsy, the diet has also been used with varying degrees of success in the areas of Alzheimer’s disease, Parkinson’s disease, autism and several other neurological conditions.
What Is A Ketone Body? – Explained by Diana Reid, MPH, RD
What A Medically Directed Keto Diet Looks Like
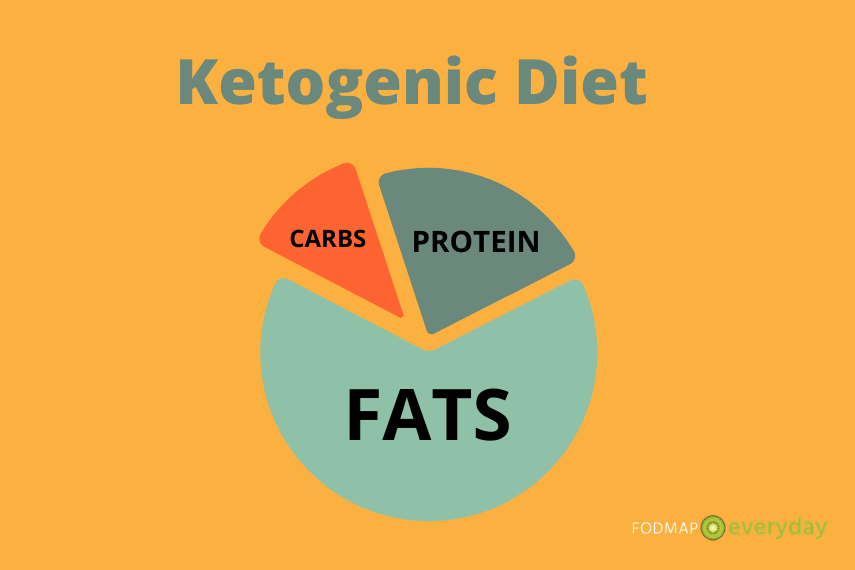
The CKD in its medical form, consists of varying ratios of fat intake to carbohydrate plus protein intake.
For example, a 4:1 ketogenic diet is quite extreme and would provide an individual with 90% of their daily calories from fat and 10% from carbohydrates and protein combined. For a young child who is eating 1100 calories per day, this would amount to 110 grams of fat, 11 grams of carbs and 17 grams of protein.
A day’s menu for this dietary prescription would look like this:
- Breakfast: 40g heavy cream, 32g sausage links, 24g avocado, 5g canola oil
- Lunch: 40g heavy cream, 18g sliced turkey breast, 22g sliced celery and cucumber, 22g mayonnaise
- Dinner: 40g heavy cream, 20g baked cod, 43g roasted cauliflower, 23g butter
- Snack: 10g strawberries, 28g whipped heavy cream.
As you can see, this type of diet is very clearly deficient in many nutrients due to the high fat content and requires children on the diet to take multiple supplements to maintain overall nutritional status and avoid adverse side effects, such as stunting or growth delays, bone loss, gastrointestinal issues, kidney stones, pancreatitis, hypoglycemia, acidosis and others.
When prescribed in this manner, it is highly supervised by physicians and dietitians and is intended to be a temporary treatment that is implemented for 1-2 years and then discontinued or reduced in intensity.
Why do I share this with you? Because the current Internet version of the “ketogenic diet” is most likely not actually a ketogenic diet, and thus we cannot expect consistent results.
The “Modern-Day” Ketogenic Diet
Somewhere in the early 2010s, once the Paleo diet started losing steam, the ketogenic diet (“keto”) began to emerge as the fad diet du jour.
The keto diet is now touted as useful for managing conditions such as obesity, autism, diabetes, hypertension, hyperlipidemia and more. However, despite its rampant popularity, it’s important to note that at this time there are no evidence-based guidelines to adapt a ketogenic diet for weight loss, diabetes, hypertension, elevated cholesterol or IBS.
This may be for several reasons, including:
- There is no standardized version of “keto,”which means you’ll see carbohydrate recommendations varying from 20-100 grams per day, relatively high protein intakes and/or supplementation with “ketone esters” to add extra ketones from beverages or pills.
- Most individuals are likely not in ketosis (see #1 above) and over-the-counter measurement of ketones (via urine strips) is highly variable. The gold standard for measuring ketone levels is via the blood rather than urine.
- The mere presence of ketones in our blood or urine doesn’t mean that they are doing magical work. In fact, all of us will have some ketones in our urine after a long fast or period of very low food intake, prolonged exercise, or sometimes just by waking up in the morning. This is a natural process to help our body avoid shutting down due to starvation. It is not indicative of healing of any kind.
- Related to #3 above, there’s very little evidence to date that tells us what ketone levels in our body are required to have positive impacts on neurological or metabolic issues. In the intractable epilepsy world, there are guidelines for “target therapeutic levels,” however this doesn’t exist for weight loss, metabolic issues or sports performance. We simply don’t know what the “right” number of ketones are, if any.
- A true ketogenic diet can be challenging to follow in the long-term as it offers limited choice in fruits and vegetables, few options for grains or seeds, and includes a high degree of fat, which isn’t always super palatable. Thus, any possible results are likely fleeting or inconsistent.
You May Want To Read: Don’t Fall For These 5 IBS Diet Fads!
IBS & the Ketogenic Diet: Lots of Cons, Not Many Pros
Now that we’ve explored the ins and outs of the ketogenic diet, let’s look at it as applied to IBS. In reality, a diet rich in fat is likely to exacerbate rather than reduce IBS symptoms and may cause adverse impacts nutritionally. Let’s take a look at why this is:
High fat foods trigger the secretion of cholecystokinin (CCK), a gut hormone that stimulates fat and protein digestion, promotes the sensation of fullness, and delays gastric emptying.
IBS sufferers already have an overproduction of CCK, therefore eating a very high fat diet may worsen symptoms.
- Several studies demonstrate high fat intake from either food or direct infusion into the duodenum (the first part of the first part of the small intestine) via a feeding tube results in delayed gastric emptying, abdominal pain, gas retention, and distention.
- A high fat meal can trigger a strong gastrocolic reflex that stimulates contractions in the large intestine to make room for more food, often resulting in an urgent bowel movement soon after eating. For individuals with IBS-D this is likely the last thing they need.
- Sometimes IBS sufferers have overlapping gastrointestinal-related diseases such as inflammatory bowel disease (IBD). When villi in the small intestine are inflamed, they do not receive the proper signals to produce lipase (the enzyme that helps breakdown fat) resulting in fat malabsorption – diarrhea; steatorrhea; deficiencies in fat-soluble vitamins, such as A, D, E and K and foul-smelling stools.
- A high fat diet may be less tolerated by SIBO (small intestinal bowel overgrowth) sufferers, because the colonic bacteria that have taken up residency in the small bowel can disrupt and inactivate bile acids, resulting in fat malabsorption and increased symptoms.
- A low carbohydrate diet offers very little fiber. It is very challenging to consume the daily recommended intake of 25-35 grams of fibers per day on a ketogenic diet, likely worsening symptoms for those with IBS-C and leaving individuals at risk for additional gut dysfunction.
- Several human based trials indicate a decrease in diversity of gut bacteria when on a ketogenic diet for six months secondary to low fructan intake. Over-restricting one’s diet to exclude or greatly reduce fruit, legumes, starchy vegetables, and other prebiotic fibers can negatively affect the healthy balance of your gut microbiome. Supplementation with pre- and probiotics is encouraged if one adapts this dietary pattern.
- Low intake of foods rich in Vitamin D, calcium, and B vitamins, increasing risk of deficiencies of these nutrients.
- High intake of saturated fat, which has been shown to increase insulin resistance. This is clearly not ideal for either weight reduction or healthy carbohydrate metabolism.
- Additionally, anyone who suffers from IBS and another health issue, such as high cholesterol, kidney disease, gallbladder issues or pancreatic concerns, should not undertake the ketogenic diet as the diet would be likely exacerbate these conditions as well.
The Ketogenic Diet & Weight Loss
The modern-day keto diet is extremely popular in diet and fitness circles, and a number of studies have touted its effects for rapid weight loss.
This rapid weight loss is the result of the body using up its stores of glucose (called glycogen) due to the lack of carbohydrate intake. Every gram of glycogen is stored in the body with three grams of water, thus as glycogen is eliminated so is water.
The number on the scale changes rapidly, which can be exciting for the dieter, but the resulting weight is mostly fluid. Once the body runs out of stored glycogen weight loss generally slows, and the process of fat loss is then generally equivalent to that of other diets over the longer term, including a low-fat diet, a very low-calorie diet, intermittent fasting and/or other weight loss diets.
In general, most weight loss diets can lead to a short-term reduction in weight, however they tend to be unsustainable over periods of longer than one to two years and studies have shown that most weight is eventually regained (usually with additional weight).
Therefore, the best “diet” is one that is diverse and filled with plenty of fruits, vegetables, whole grains, legumes, nuts and seeds, fish and lean meats.
Watching portion sizes, reducing intake of highly processed foods and increasing physical activity can all be helpful in ensuring a healthy body. Individuals with specific health issues, such as diabetes may benefit from a low carbohydrate or keto diet for blood sugar management and weight control, but in most situations, a balanced diet is the ideal middle ground.
You May Want To Read: Weight Management Series: How to Lose Weight on the Low FODMAP Diet and Weight Management Series: How to Gain Weight on the Low FODMAP Diet
The Takeaway
Is There a Situation Where the Ketogenic Diet Would Help IBS Sufferers?
Perhaps. The reduction in carbohydrates from a ketogenic diet can help temporarily ease gut issues such as gas, bloating, abdominal pain and diarrhea or constipation, because such a diet reduces the total load of fermentable carbohydrates (FODMAPs) that can cause these same symptoms. Thus, some individuals may feel better in the short term on keto. However, cutting out almost all carbohydrates tends to throw the proverbial baby out with the bathwater. Some carbohydrates, especially prebiotics, have important effects on our gastrointestinal tract and our overall health.
[bctt tweet=”However, cutting out almost all carbohydrates tends to throw the proverbial baby out with the bathwater. Some carbohydrates, especially prebiotics, have important effects on our gastrointestinal tract and our overall health.” username=”FODMAPeveryday”]
Reducing these carbohydrates can also reduce bacterial abundance and diversity in our gut, leaving us vulnerable to rogue bacteria that can cause inflammation or infection.
A better treatment strategy might be to undertake the low FODMAP diet temporarily to reduce the overall FODMAP load (and decrease symptoms), while also optimizing overall nutrition and reducing the risk of any additional health challenges. Finding a middle ground between “all carbs are bad” and “some carbs are problematic” is likely the healthiest path to take.
NOTE: As always, work with your doctor and/or dietitian to develop a customized treatment plan (diet, lifestyle, medication) that works best for you. You are unique.
References:
- D’Andrea Meira I, Romão TT, Pires do Prado HJ, Krüger LT, Pires MEP, da Conceição PO. Ketogenic Diet and Epilepsy: What We Know So Far. Front Neurosci. 2019;13:5. Published 2019 Jan 29. doi:10.3389/fnins.2019.00005
- Charlie Foundation. (2019). What is a Ketogenic Diet? Keto Diet Facts, Research, and Variations. [online] Available at: https://charliefoundation.org/diet-plans/ [Accessed 21 Jul. 2019].
- Epilepsy Foundation. (2019). Side Effects on the Ketogenic Diet: Identification and Treatment. [online] Available at: https://www.epilepsy.com/article/2007/11/side-effects-ketogenic-diet-identification-and-treatment [Accessed 21 Jul. 2019].
- Sanjay Kalra, Rajiv Singla, Rahul Rosha, Munish Dhawan. Ketogenic diet: situational analysis of current nutrition guidelines. Journal of the Pakistan Medical Association, Volume 68, Issue 12. December 2018
- Dhillon KK, Gupta S. Biochemistry, Ketogenesis. [Updated 2019 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493179/
- Magnus Simrén, Hasse Abrahamsson, Einar S. Björnsson. Lipid-Induced Colonic Hypersensitivity in the Irritable Bowel Syndrome: The Role of Bowel Habit, Sex, and Psychologic Factors. Gastroenterolgy and Hepatology. Volume 5, Issue 2, Pages 201–208. February 2007.
- Jackson A, Lalji A, Kabir M, et al. The efficacy of a low-fat diet to manage the symptoms of bile acid malabsorption – outcomes in patients previously treated for cancer. Clin Med (Lond). 2017;17(5):412–418. doi:10.7861/clinmedicine.17-5-412
- com. (2019). CPE Monthly: Small Intestinal Bacterial Overgrowth – Today’s Dietitian Magazine. [online] Available at: https://www.todaysdietitian.com/newarchives/070115p50.shtml [Accessed 21 Jul. 2019].
- Sofia Reddel, Lorenza Putignani,and Federica Del Chierico. Impact of Low-FODMAPs, Gluten-Free, and Ketogenic Diets on Gut Microbiota Modulation in Pathological Conditions. Nutrients. 2019 February 12;11(2)
- Wan, Y., Wang, F., Yuan, J., Li, J., Jiang, D., Zhang, J., Li, H., Wang, R., Tang, J., Huang, T., Zheng, J., Sinclair, A., Mann, J. and Li, D. (2019). Effects of dietary fat on gut microbiota and faecal metabolites, and their relationship with cardiometabolic risk factors: a 6-month randomised controlled-feeding trial. Gut, 68(8), pp.1417-1429.
- Luukkonen, P., Sädevirta, S., Zhou, Y., Kayser, B., Ali, A., Ahonen, L., Lallukka, S., Pelloux, V., Gaggini, M., Jian, C., Hakkarainen, A., Lundbom, N., Gylling, H., Salonen, A., Orešič, M., Hyötyläinen, T., Orho-Melander, M., Rissanen, A., Gastaldelli, A., Clément, K., Hodson, L. and Yki-Järvinen, H. (2018). Saturated Fat Is More Metabolically Harmful for the Human Liver Than Unsaturated Fat or Simple Sugars. Diabetes Care, 41(8), pp.1732-1739.
- Dieting does not work, UCLA researchers report. (2019). Retrieved 15 November 2019, from https://newsroom.ucla.edu/releases/Dieting-Does-Not-Work-UCLA-Researchers-7832
- Gardner, C., Trepanowski, J., Del Gobbo, L., Hauser, M., Rigdon, J., & Ioannidis, J. et al. (2018). Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association With Genotype Pattern or Insulin Secretion. JAMA, 319(7), 667. doi: 10.1001/jama.2018.0245
- Aragon, A.A., Schoenfeld, B.J., Wildman, R. et al.International society of sports nutrition position stand: diets and body composition. J Int Soc Sports Nutr 14, 16 (2017) doi:10.1186/s12970-017-0174-y
- Kirkpatrick, C., Bolick, J., Kris-Etherton, P., Sikand, G., Aspry, K., & Soffer, D. et al. (2019). Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. Journal Of Clinical Lipidology. doi: 10.1016/j.jacl.2019.08.003







Learned some new stuff with very detailed information.
Sigh. Lots of FUD here:
>Why do I share this with you? Because the current Internet version of the “ketogenic diet” is most likely not actually a ketogenic diet, and thus we cannot expect consistent results.
There are certainly good and bad ketogenic diets. Most people end up reasonably close to a whole food diet simply because most processed foods are not keto-compatible. Just like somebody could eat a lot of gluten-free pasta or a lot of hard cheese on a FODMAP diet.
> it’s important to note that at this time there are no evidence-based guidelines to adapt a ketogenic diet for weight loss, diabetes, hypertension, elevated cholesterol or IBS.
So, the virta health diabetes trials provide no evidence of efficacy for keto on type II diabetes?
Hi Eric, this is Diana’s response. Thank you for being patient: Hi Eric, thanks for your comment. It is true that there are good and bad dietary patterns of all varieties. Our aim is not to “bash” any particular diet, but to show the pros and cons, as well as any potential nutritional ramifications from excessive food restrictions, as we feel this article did. It is true that science is always evolving, and newer studies regarding a ketogenic diet for certain health concerns is increasing, however the body of evidence is what we tend to emphasize in our articles, versus a few smaller studies here and there. The Virta stuff is interesting certainly, but in our view, the studies are quite limited in terms of both numbers of participants and long-term timeframes. So, while we will watch them with interest, we stand by our current article.