Will Enzyme Supplementation Help With Gas and Bloating?
As an Irritable Bowel Syndrome (IBS) sufferer, you may have tried just about every possible combination of food, beverage and supplements, hoping for relief.
You may have heard of or read about digestive enzymes and wondered if they can help you. But, randomly trying yet another supplement and hoping for the best can be a painful road to travel.
So, what’s a bloaty, gassy person to do? Behold: Your primer on digestive enzymes and IBS!
What Are Digestive Enzymes?
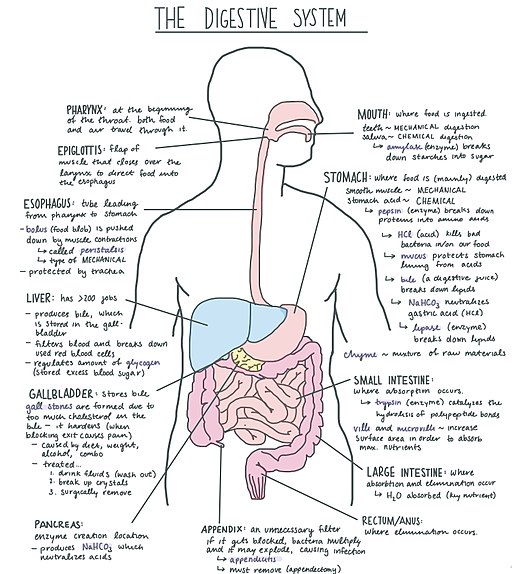
Most individuals produce a variety of enzymes in their digestive tract that help them to digest the food they eat.
For example, the saliva produced in your mouth contains an enzyme called amylase, which starts to break down starch into simple sugars as you chew your food.
Further on down the line, your stomach produces the enzymes pepsin and gastric lipase, which help to break down protein and fat into smaller components that can be absorbed by your small intestine.
Your pancreas also produces additional digestive enzymes (amylase, lipase, proteases) that break down starches, fats and proteins into smaller parts that can be absorbed and turned into fuel for your body and its daily activities.
What Happens If You Don’t Have Enough Digestive Enzymes?
Some individuals may not produce sufficient enzymes to aid in proper digestion. For example, many people of East Asian, African, or Latin American descent lose the ability to digest lactose as they mature (called lactase nonpersistence).
Individuals with poorly managed celiac disease may also have problems digesting lactose as a result of damage to their intestinal villi, which normally produce lactase.
Individuals with pancreatic or gallbladder disease may suffer from digestive issues related to deficiency of enzymes produced or stored by these organs.
Finally, some individuals with hereditary or genetic mutations may also lack or have very limited production of certain digestive enzymes.

You May Want To Read: What Conventional Wisdom Gets Wrong About Bloating
The Connection Between IBS, FODMAPs & Digestive Enzymes
In order for the body to digest certain nutrients, they must be broken down from complex molecules into smaller, discrete components, which can then be absorbed into the small intestine and circulated through the body. In the case of FODMAPs, there are several hurdles that may get in the way of proper breakdown and digestion due to the chemical structure of these FODMAP sugars.
You May Want To Read: All About Disaccharides
Digesting The “D” In FODMAPs
For example, lactose, the disaccharide found in dairy products, is comprised of the sugars glucose and galactose. As noted above, insufficient production of the lactase enzyme inhibits this process and allows the lactose to pass unabsorbed from the small intestine to the colon where trillions of bacteria are ready and willing to consume and ferment them, leading to symptoms of gas and bloating.
And, because these large bits of lactose alter the fluid equilibrium of the colon (they are considered “osmotic”), additional fluid is pulled in to try to balance things out; causing diarrhea and further sloshy discomfort.
Digesting The “O” In FODMAPs
Similarly, fructans, polysaccharide chains of fructose sugars joined together with a glucose molecule at the end, must be broken down into these component sugars to be fully digested. However, humans do not actually produce a digestive enzyme that can break the bonds between these fructose and molecules and their glucose buddy, so once again these larger molecules are moved along to the colon, where certain bacterial species — bifidobacteria and Lactobacillus — produce the 2,1-β-d-fructan-fructanohydrolase enzyme, allowing these colonic bacteria to hydrolyze or break them apart. Examples of fructans include wheat, onions, garlic, and leeks.
Galactans, like fructans, are also complex molecules, consisting of chains of galactose bound together with glucose at the end of their structure. Again there is no human-produced enzyme able to break these into smaller pieces for proper digestion, so galactans are passed along to the large intestine mostly whole. Examples of foods in this category include lentils, beans, chickpeas, broccoli, and soy.
Your Body Is A Transportation System
In the case of fructose digestion, it is less an issue of enzyme production and more a challenge of transport. While fructose is a monosaccharide (meaning it is not comprised of different sugars joined together), in order be properly and completely digested it needs to be carried across the walls of the small intestine by a transporter. This transporter mediated facilitated diffusion is the equivalent of the digestive buddy system. In fructose’s case, the GLUT-5 transporter must be available in sufficient quantities to properly escort fructose into the bloodstream.
If there’s more fructose available than seats on the GLUT-5 bus, this excess fructose escapes small intestinal digestion and moves on to the colon, once again causing uncomfortable symptoms from fermentation and high osmotic load. Interestingly, if glucose is also along for the ride, it can help support the digestion of fructose, as long as glucose is present in higher amounts than fructose.
Thus, fructose intolerance isn’t necessarily about an inability to absorb fructose, it’s an issue of excess fructose as compared to glucose. Foods with excess fructose include mango, honey, agave syrup, watermelon, apples, and pears.
How Might Enzyme Supplementation Help with Digestion and Enhanced FODMAP Tolerance?
As discussed above, an insufficiency or outright lack of digestive enzymes can lead to unpleasant symptoms, especially for individuals with visceral hypersensitivity. Digestive enzyme supplementation has become increasingly popular in the gut health field. However, scientific data remains limited, as most individuals have different tolerance levels and there is no current universal recommended “dosage” to aid in digestion. Production processes may also differ widely, leading to inconsistent quantity or quality of enzymes, depending on the manufacturer.
However, given some of the nutritional complexities of the low FODMAP Diet and the potential for over-restriction, nutrient deficiencies or gut dysbiosis, the addition of supplemental digestive enzymes may allow individuals to eat a larger variety of nutritious foods while still experiencing reduced symptoms.
Let’s take a look at what enzymes are available and how they might help with digestion of FODMAPs.
- alpha-galactosidase: This enzyme helps break down certain oligosaccharides (the “O” in FODMAPs). It tends to be most active in breaking down raffinose and stachyose, galacto-oligosaccharides (GOS) found in beans, peas, cabbage, some whole grains, broccoli, and some other vegetables. There have been claims by manufacturers that this enzyme may also help break down fructans into its component parts, however research has yet to substantiate this.
- Lactase (B-galactosidase): This enzyme helps break down lactose (the “D” in FODMAPs) into its component sugars; glucose and galactose.
- Fructan hydrolase: Used often in the food manufacturing industry and produced by bacteria, this enzyme can be helpful in breaking apart the fructosidic bonds found in inulin and other fructan subtypes (one of the “O’s” or oligo-saccharides in FODMAPs). Fructan hydrolase thus reduces fructan to fructose, glucose, and inulooligosaccharides, which may be easier to digest for some individuals.
It’s important to note that a wide-spectrum fructan hydrolase may be able to tackle various types of fructan – beyond inulin – that exist in food. A particular type of fructan hydrolase, inulinase, may be more limited in its application, as it only claims to target inulin.
- Xylose Isomerase: Another enzyme that isn’t produced by the human body, this enzyme can help break down fructose into glucose molecules, which can improve digestion and absorption of the “M” (for monosaccharide) in FODMAPs.
- Pancrealipase: This enzyme breaks down dietary fat (triglycerides) into smaller particles. It is important to note that dietary fat is not a FODMAP, however some IBS sufferers do struggle with digestion of high fat meals, so this enzyme may be a useful adjunct in some cases.
- Amylase: While not considered a FODMAP, certain individuals may struggle to digest resistant starch, large amounts of which can be found in foods that have been cooled and then reheated, such as pasta, potatoes, or rice. It’s also found in oats, lentils, corn and corn starch, green bananas, and some nuts and seeds. Amylase supplementation is thought to help reduce gas and bloating caused by the gut fermentation of resistant starch.
| Enzyme/Product | What To Take | Where To Buy | How To Use |
|---|---|---|---|
| alpha-Galactosidase | Beano is a common supplements of this type in the U.S. *Beano caplets contain mannitol and/or sorbitol. Read labels carefully! | Beano and other alpha-galactosidase supplements are available via Amazon or other pharmaceutical retailers. | Look for a supplement that contains 300 GALU. Take one caplet with the first bites of your meal that contains GOS. |
| Lactase | Lactase enzyme supplements are commonly available in caplets and drops (and is already added to lactose-free dairy products). *Lactaid original strength caplets contain mannitol. Avoid this product if you are sensitive to this FODMAP or choose the Lactaid Fast Act caplets instead. | Widely available in pharmacies, some grocery stores and online retailers. | Take 1-3 tablets per meal or add 5-15 drops to one liter of milk and refrigerate for 24 hours before using. Adjust to your own personal tolerance levels |
| Xylose Isomerase | Xylosolv and Fructosin are two brand names of XI, but this supplement is not widely available in the U.S., except mixed with other enzymes, which may contain added pre- and probiotics. *Read labels carefully to avoid high FODMAP ingredients. | Check for online retailers and/or ask your pharmacy. | Take 1-2 capsules with liquid before high fructose-containing meals. |
Enzyme Products: Single Or Combo?
Current products available on the market to aid in digestion of FODMAPs include several combination enzymes, as well as individual such as:
- Kiwi Biosciences‘ FODZYME ® contains alpha-galactosidase, lactase, and wide-spectrum fructan hydrolase. It is Monash University lab tested and certified low FODMAP. You can read more in our interview with the brand founders.
- Intoleran offers Quadrase Forte (for multiple FODMAPs), Lactase, Fibractase (alpha-galactosidase), Fructase (xylose isomerase) and Starchway (gluco-amylase and invertase) products.
- Microbiome Labs FODMATE – contains alpha-galactosidase, glucose isomerase, lactase, inulinase and pectinase.
- Other individual enzymes are also available, typically online or via your local pharmacy (see the Supplemental Table above for additional details).
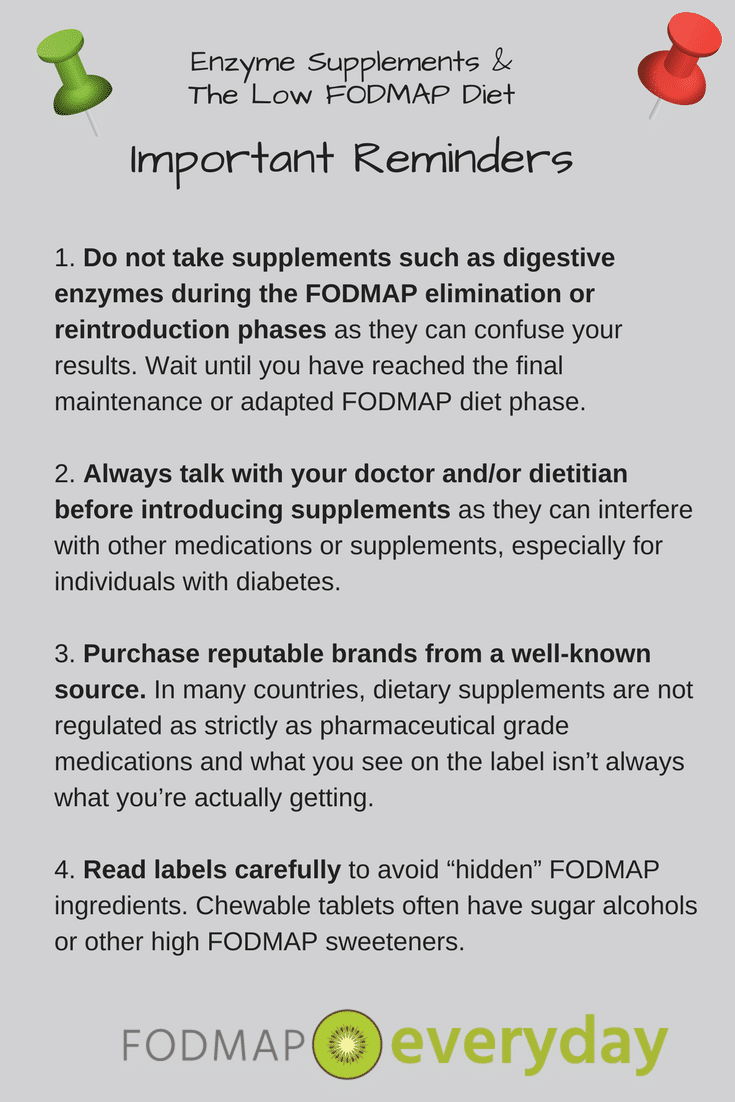
How to Take Digestive Enzymes
It’s recommended to complete all three phases of the low FODMAP diet before introducing digestive enzymes. The Challenge Phase will help you identify which FODMAPs are the most problematic for you, allowing you to then experiment with using enzymes to extend your tolerance level for certain foods.
Take the products according to package directions (generally 1-3 capsules at the start of a meal) and note both the quantity of enzymes taken and the quantity or type of FODMAPs consumed. This can help you adjust enzyme supplementation up or down as appropriate.
Most enzyme supplements come in multiple “strengths” (e.g., the number of units of enzyme per capsule or tablet), so depending on your own level of tolerance, you may wish to start higher or lower in dosage to properly manage your symptoms and/or to correspond to the level of FODMAPs in any given meal.
The research team behind FODZYME®, however, found that it’s critical for enzymes to distribute within the ingested food while the stomach pH range is optimal for enzymatic activity. This is why FODZYME® comes in powder form, which facilitates maximum enzyme integration in food, allowing the enzymes to swiftly target FODMAP triggers in a meal.
The makers of FODZYME explain how to take their enzyme at meal time in this video:
Do They Work?
Anecdotally, in the clinical setting, I have found that digestive enzymes can provide significant relief for some individuals, but may also result in no change in symptoms for others.
Results may vary depending on the supplement used and the intolerance(s) targeted. For example, a supplement that breaks down fructans may help with digestion of oligo-saccharides, but may also lead to greater symptoms if the individual is intolerant to fructose (because fructans will be broken down into fructose and glucose) and there is no xylose isomerase present in the product used, such as with Intoleran’s Quadrase products. Thus, it is important to work with your dietitian to identify the right enzyme combination for you.
It is important to work with your dietitian to identify the right enzyme combination for you.
In terms of scientific research, there is some useful yet limited evidence regarding effectiveness for digestive enzymes in IBS symptom relief. For example, a 2017 study by Tuck et al [2] found that in GOS-sensitive IBS patients, alpha-galactosidase (AG) supplementation led to a significant reduction in abdominal pain, bloating and overall IBS symptoms, while a 2015 study by Finnish researchers [3] was not as positive. This older study concluded that while there was a trend toward reduced symptoms with the AG supplementation, regular supplementation was not recommended.
So, what to do? In this case, individuals who know that they are GOS-sensitive may want to trial supplementation of AG to see if it helps reduce symptoms. Supplementation with this enzyme may also be useful for individuals who follow a vegan or vegetarian version of the low FODMAP diet and have a high intake of beans and starchy or cruciferous vegetables.
When it comes to fructose malabsorption, a 2012 study [4] evaluated changes in hydrogen production between two study groups. One group took a placebo, and another took xylose isomerase (XI).
Each group ingested a relatively large dose of fructose and then completed hydrogen breath tests at 0, 30, 60, 120, 180 and 240 minutes. The group that took the XI showed lower production of hydrogen and reduced symptoms of abdominal pain, bloating and nausea, which is promising.
However, it is important to note that these patients had only very mild symptoms at baseline, so it is difficult to know if more severe symptoms would be positively affected. A more recent double-blind, placebo-controlled study also showed a significant decrease in breath hydrogen with intake of xylose isomerase after ingestion of fructose, and significant improvement of both nausea and abdominal pain.
More Studies Are Needed
In vivo (human studies) evaluating the effectiveness of inulinase in increasing digestibility of inulin-type fructans are extremely limited, however food industry studies have shown some significant promise.
A 2020 publication reported that extracted fructans (from wheat, inulin, FOS or lentils/GOS) treated with a combination of insulinase, alpha-galactosidase and invertase showed significant reduction in fructan concentration, however the timing and degree of fructan degradation varied considerably.
Additionally, the byproducts of this fructan breakdown also varied, with excess fructose being produced in the largest quantities by inulinase in the wheat extract, and insulinase and invertase producing excess fructose in the tested lentil flour. It’s hard to know exactly how this experiment would translate to real foods in a living digestive system, and the generation of excess fructose from fructan breakdown may lead to one malabsorption issue being resolved and another created, so additional research will be needed to assess the usefulness of these enzymes as a significant digestive aid.
Kiwi Biosciences performed a series of in-vitro experiments to validate the activity of the fructan hydrolase enzyme and discovered that, when FODZYME® was administered, fructan was rapidly broken into simple fructose and glucose with ~90% of the fructan degraded within 30 minutes.
Pancreatic lipase was studied in a small 2010 pilot study on post-meal IBS-D, where it was found useful in reducing symptoms of cramping, bloating, pain and urge to defecate, while increasing stool firmness. This particular study was sponsored by a pharmaceutical company, which provided the pancrealipase for study participants. Another recent study by Nishiyama et al showed that supplementation of pancreatic lipase in mice increased the quantity of a key beneficial bacteria in the intestinal tract, however it has not been studied in humans. Thus, the data is somewhat unclear.
Lactase supplementation has been studied and used for decades and has been proven to be helpful for individuals with mild to moderate lactose intolerance. Supplementation does not always eliminate (convert) 100% of the lactose, so individuals who are extremely lactose sensitive may wish to avoid all naturally occurring lactose-containing products and/or choose products that are clearly labeled “lactose free.”
The Takeaway
Digestive enzymes may be a helpful tool in your IBS-fighting arsenal and may allow you to increase quantities of certain foods or reintroduce others, aiding in reduced dietary restriction and increased nutritional density. Talk with your dietitian about if, how and when to incorporate them into your dietary routine.
This article generously sponsored by:
You May Want To Read: FODZYME- Digestive Enzymes to Help with IBS
References
[1] Emedicine.medscape.com. (2018). Lactose Intolerance: Background, Pathophysiology, Etiology. [online] Available at: https://emedicine.medscape.com/article/187249-overview#a6 [Accessed 1 Mar. 2018].
[2] Tuck, C., Taylor, K., Gibson, P., Barrett, J. and Muir, J. (2018). Increasing Symptoms in Irritable Bowel Symptoms With Ingestion of Galacto-Oligosaccharides Are Mitigated by α-Galactosidase Treatment.
[3] Markku Hillilä, Martti A. Färkkilä, Taina Sipponen, Janne Rajala & Jari Koskenpato (2015) Does oral α-galactosidase relieve irritable bowel symptoms?, Scandinavian Journal of Gastroenterology, 51:1, 16-21, DOI: 10.3109/00365521.2015.1063156
[4] Komericki, P., Akkilic-Materna, M., Strimitzer, T., Weyermair, K., Hammer, H. F. and Aberer, W. (2012), Oral xylose isomerase decreases breath hydrogen excretion and improves gastrointestinal symptoms in fructose malabsorption – a double-blind, placebo-controlled study. Aliment Pharmacol Ther, 36: 980–987. doi:10.1111/apt.12057
[5] Money ME, Walkowiak J, Virgilio C, et al. Pilot study: a randomised, double blind, placebo controlled trial of pancrealipase for the treatment of postprandial irritable bowel syndrome-diarrhoea, Frontline Gastroenterology 2011;2:48-56.
[6] Nishiyama H, e. (2018). Supplementation of pancreatic digestive enzymes alters the composition of intestinal microbiota in mice. – PubMed – NCBI. [online] Ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/pubmed/29106956








Finally a comprehensive breakdown of the enzyme FODMAP maze with science!!
Thank you!
I have found that the Eat Anything RX digestive enzyme, available on Amazon, works perfectly in fructose and lactose digestion. The manufacturer claims that it also helps digest legumes but have not tried it yet for this purpose.
The digestive enzyme Lypo Gold, manufactured by Enzymedica and also available on Amazon, works perfectly in fat digestion at 1/20th the cost of Zenpep, a prescription drug recommended by my gastroenterologist.
Hello Carol! Thank you for writing. We will forward this to the author, Diana, and have her respond.
Dédé
Can’t seem to get this in England -any tips?
What kind of enzyme are you looking for in particular? What symptoms are you addressing?
Thanks for the great suggestion for the Eat Anything RX supplement Carol! It does look like it has enzymes for lactose, excess fructose and galacto-oligosaccharides. The dose to take will depend on which FODMAPs you are most sensitive to. Some individuals may not need all 3 enzymes in one supplement, depending on FODMAP tolerance/sensitivity, so a single enzyme supplement may work better for those individuals.
The other supplement you mentioned contains enzymes that haven’t necessarily been scientifically tested specifically for IBS. They may help some individuals, but may not be useful for others.
As always, it’s best to speak to your doctor or dietitian before taking a new supplement.
Hello and thank you SO much for this article!!! Wish I had had this info years ago. Question though: why put mannitol in Beano when we cannot manage it for IBS? Why not just sugar or Stevia that would not be dangerous to us? Now in saying that, I have been on Beano for two weeks and have not had any D at all!! This is a record for me and I’m enjoying eating more food. I’m on a modified lofo diet (from my GI and RD) but still had symptoms every week and daily nausea. All those symptoms are greatly reduced or gone!! .
Hi Angela, we are so happy that the article was helpful! As you read, different supplementation is geared at various digestive complaints – not all of them FODMAP related, hence mannitol cropping up. BUT the great news is that you are finding your way! Here is to your continued digestive success!
Hello. I am having a difficult time determining what might be causing my unremitting bloating. One of the reasons for this might be because I have no other symptoms, none. Even when I am not in a cycle of severe bloating, I always seem, however, to be somewhat bloated no matter what I eat. I have tried excluding foods that might bloat me from my diet, to avail. I exercise and eat only whole foods; no sugar and no junk. If someone could be kind enough to offer some insight on this problem, I would greatly appreciate it, as I have just about exhausted all avenues open to me. I have tried consulting with doctors, but they know close to nothing about my problem because I have no other symptoms. I am going to try supplementation with digestive enzymes and see if I can reduce the severity of this cycle. Good luck to all of you out there in achieving what we are all striving for: stomach health!
Hi Andres, I am so sorry you are going through this – but know you are not alone. It is not unusual for doctors, even gastroenterologists to not be the best at working with patients to get to root issues. However, Registered Dietitians ARE FANTASTIC at this and one of the reasons we see people achieving success when they work with a RD, as opposed to when they don’t. Also, BTW, it is not recommended that you necessarily dive in with supplementation until you get medical, such as that from a RD. You might take a look at our article that discusses the difference between Dietitians and Nutritionists and also our article on Tamara Duker Freuman, who is affectionately referred to as The Bloated Belly Whisperer. Her book is Amazing and focuses on bloating.
Hello. The article notes that alpha-galactosidase and xylose isomerase are not produced by our bodies. 1) Are these a natural component of any foods, and if so, which? If not, what research as been done regarding their safety? 2) The article doesn’t say whether our bodies produce pancrealipase. Please clarify, and if we don’t, I have the same question about safety research regarding pancrealipase.
On a separate matter, I am hoping that manufacturers catering to people who need low-fodmap products will start offering enzymes and other products that are low-fodmap friendly by leaving out mannitol and other known triggers.
I recently discovered your site. It’s GREAT! Thank you!
Hi Ann. The RD who wrote the article is on break and we will get back to you as soon as we can. Thank you for writing and we are so glad you have joined our community.
I have tremors! Difficult to text! Information about more extreme symptoms/reactions, rapid heart rate, flushing, exaggerated tremors, etc. Is there a number to call for those who have difficulty texting?
Hi Audrey, we do not offer medical advice.