Fructose intolerance affects up to 40% of the adult population. Could this be a dietary trigger for you?
When it comes to carbohydrate intolerances, you’ve probably already heard of lactose intolerance. And for good reason—nearly 70% of the global population malabsorbs milk sugar due to a deficiency in the lactase enzyme. 1
But have you heard of fructose intolerance? If not, you may be surprised to learn that fructose—the primary sugar in honey, fruit juice, and high-fructose corn syrup—can be malabsorbed by all humans. Yes, fructose consumed in excess amounts can cause digestive trouble for all of us.
As mentioned, up to 40% of adults are estimated to have a particularly limited ability to absorb fructose 2, which can routinely lead to uncomfortable gastrointestinal symptoms two to eight hours after consuming a high-fructose food or drink. This simple sugar has quickly gained attention as a possible trigger for symptoms of irritable bowel syndrome (IBS), and fructose reduction may be a helpful treatment for some.
In addition to dietary fructose intolerance, a rare genetic disorder exists that also requires fructose avoidance, but in a stricter form.
- What The… Fructose?
- “Fructose Intolerance” Can Have Two Different Meanings
- Where Does Fructose Go Wrong?
- Heredity Fructose Intolerance (HFI) is a Medical Condition
- Testing for Dietary Fructose Intolerance
- The Low FODMAP Diet – A Tool for Fructose Exploration
- Fructose On the Rise
- Dietary Fructose Intolerance Symptoms – A Dose Response Relationship
- Dietary Fructose Intolerance Treatment
- High Fructose foods (Excess Fructose Foods)
- Low-Fructose Foods
- The Takeaway
What The… Fructose?
Fructose is a single sugar represented by the “M” in FODMAP which stands for “monosaccharide,” also known as simple sugars. Fructose often naturally occurs in food along with an equal or larger amount of another simple sugar called glucose. This ratio makes fructose fairly easy for the body to absorb. However, when fructose occurs without glucose, or in larger quantities than glucose, these foods are referred to as excess fructose, and can be problematic for the digestively sensitive.
You may want to read: All About Monosaccharides
A variety of fruits, vegetables, and sweeteners contain excess fructose. High fructose corn syrup also contains excess fructose and is found in commercially prepared foods, such as candy and soft drinks. (This is not the same as regular corn syrup, by the way: read more in our article Corn Syrup vs. High-Fructose Corn Syrup). Symptoms of dietary fructose intolerance can generally occur when you eat:
- Food that has relatively more fructose than glucose (e.g. watermelon)
- Pure fructose (e.g. fructose unaccompanied by glucose, such as in honey)
“Fructose Intolerance” Can Have Two Different Meanings
Unlike other carbohydrate intolerances, fructose intolerance is a term that may be used to refer to one of TWO distinctly different forms of fructose malabsorption:
1. Dietary fructose intolerance (DFI): an uncomfortable response to excess fructose, typically felt as gas, bloating, abdominal pain, and/or diarrhea, though not harmful to one’s health.
2. Hereditary fructose intolerance (HFI): a genetic inability to digest fructose which can result in organ damage if left untreated.
Luckily, both forms of fructose intolerance can be diagnosed and effectively managed with diet, though the strictness and medical necessity of the diet differs depending on whether you have HFI or DFI.
Where Does Fructose Go Wrong?
The small intestine has special cells called GLUT-5 transporters that shuttle excess fructose from the small intestine to the bloodstream. Undigested fructose molecules, also known as fructose malabsorption, can occur due to any of the following reasons:
- You have a low number of GLUT-5 transporters
- You have GLUT-5 transporters that don’t function very well
- You have sufficient GLUT-5 transporters, but have exceeded their capacity during a meal
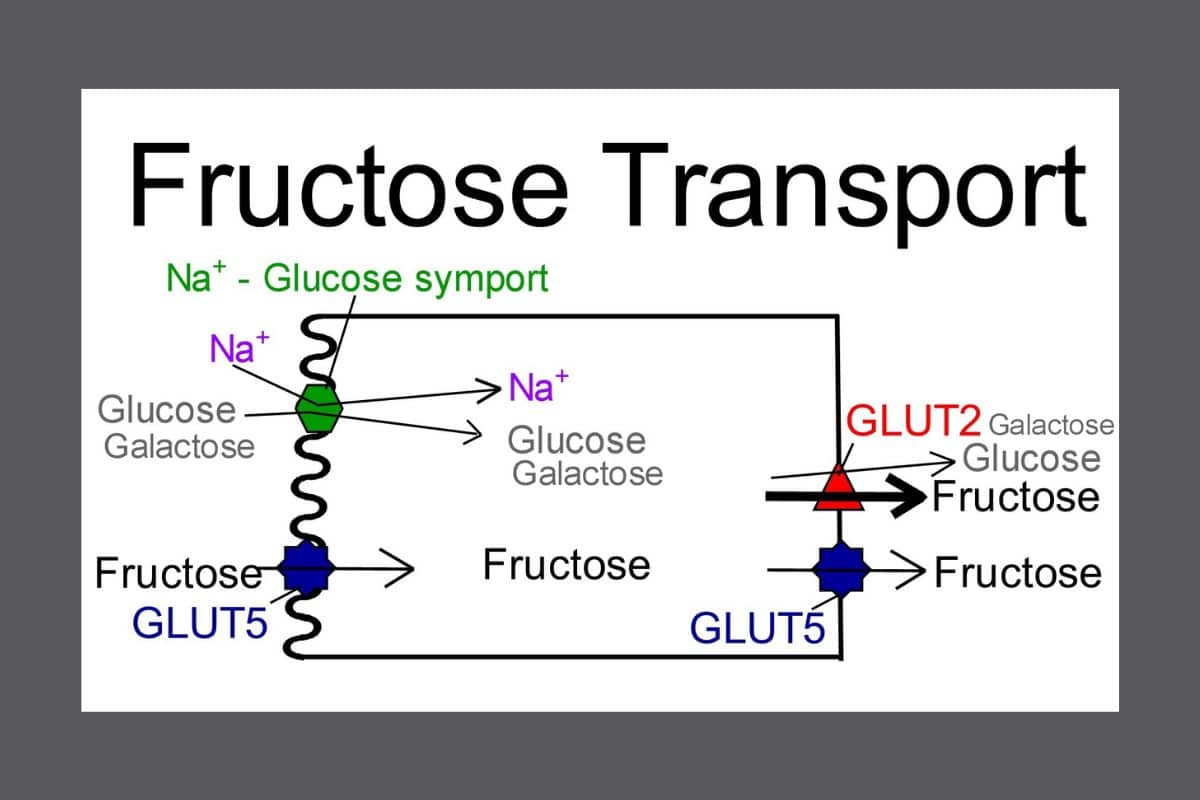
GLUT-5 transporters have a naturally limited capacity: they can get easily overwhelmed by excess fructose, which leads to malabsorption. Additionally, some people have fewer numbers of transporters OR have transporters that don’t’ function properly, which yields the same result. Unabsorbed fructose eventually ends up in the colon where it is feasted on by gut bacteria. The most common result: gas, bloating, and/or diarrhea.
In cases of hereditary fructose intolerance, the main issue is not with the transporters but with a key enzyme needed for fructose digestion. Without this enzyme, eating dietary fructose leads to a dangerous buildup of substances in the liver.
Heredity Fructose Intolerance (HFI) is a Medical Condition
Unlike dietary fructose intolerance, HFI has potentially severe health consequences. HFI is caused by a genetic mutation in the aldolase B gene, which results in an enzyme deficiency and the inability to breakdown fructose (as well as sucrose, which contains fructose). Diagnosis usually happens in infanthood once a fructose or sucrose -containing food or formula is introduced. The condition can also be diagnosed in adulthood, though less typical. Signs and symptoms of HFI may include4:
- Nausea and Vomiting
- Abdominal pain
- Hypoglycemia (low blood sugar)
- Elevated liver enzymes
- Seizures
- Jaundice (yellowing of the skin)
- Aversion to sweet foods
In people with HFI, repeated fructose consumption can cause stunted growth, liver or kidney damage, and organ failure.4 This type of fructose intolerance is treated similarly to a severe allergy: it requires very strict fructose and sucrose avoidance, since even small amounts of fructose can be damaging to the body. There is currently no supplement or medication that is an effective treatment for HFI.
Join Frusano and FODMAP Everyday As We Discuss How To Live Well With Fructose Intolerance
Testing for Dietary Fructose Intolerance
If you are suspicious of DFI, a noninvasive test called a hydrogen breath test can be used to assess absorption. This involves drinking a solution sweetened with fructose (typically 25 grams, which is roughly a can of cola) and then periodically breathing into a tube. Those breath samples are then analyzed by a machine for hydrogen and methane gases, which will indicate how much of that fructose was absorbed. If there is good digestion of the sugar, the increase in gases should be minimal. But if the fructose is poorly absorbed, we are looking for the hallmark sign of bacterial fermentation – sharp rises in exhaled gases.
There is currently no blood test to measure DFI, and food sensitivity tests that advertise carbohydrate intolerance evaluation do not actually have scientific evidence for this purpose. For a suspicion of HFI, genetic testing is most commonly used for diagnosis, not a breath test.
The Low FODMAP Diet – A Tool for Fructose Exploration
A short term low FODMAP diet can also shed light on whether you have DFI and may be especially helpful if a breath test is not planned. If there’s strong suspicion of only fructose intolerance (and not any other FODMAP categories), trying an elimination diet of fructose alone is also sometimes used.
However, many people first discover fructose intolerance on a low FODMAP diet since the Elimination Phase of the low FODMAP diet eliminates all high fructose foods, such as high fructose corn syrup, honey, and excess fructose fruits and veggies. If DFI is the main driver of your symptoms, you may feel a lot better during this phase. If symptoms return after trying high fructose food during the Challenge Phase, it’s a good clue for fructose malabsorption.
Fructose On the Rise
Changes to Western diet habits, specifically an increased reliance on processed foods with added fructose, may account for some dietary fructose intolerance symptoms. The National Health and Nutrition Examination Survey (NHANES) showed that average American intake of fructose increased by about 32 to 48% between the 1978 and 2004.3 When we pair this marked rise in fructose consumption with a sensitive, or for some, extremely limited,digestive ability, we find greater risk of fructose malabsorption and the gastrointestinal discomfort that can accompany it.
Dietary Fructose Intolerance Symptoms – A Dose Response Relationship
If fructose is a trigger of your gastrointestinal symptoms, you will most likely find that consuming more fructose will trigger worse symptoms. Fortunately, in my practice I find that most of my patients with DFI are able to land on specific portion sizes and foods that don’t cause trouble in an otherwise low-fructose meal, and can also lean on low-fructose substitutions to keep their gut happy. Companies such as Frusano specialize in fructose-free offerings.
If you are fructose-curious, a FODMAP-trained dietitian can help you assess what your fructose threshold looks like. For example, you might learn that one teaspoon of honey is a tolerable serving size, but 1 tablespoon triggers symptoms. Some trial and error is helpful to explore your sensitivity.
This experimentation is not advised for HFI, which requires avoiding even small amounts of fructose to avoid the health risks of fructose ingestion.
Dietary Fructose Intolerance Treatment
While hereditary fructose intolerance is treated through very strict adherence to a low-fructose (see below) diet, DFI can be managed through a variety of dietary strategies. This is similar to how lactose intolerance, for example, is typically handled and can involve varying combinations of the following:
- Excess fructose avoidance – eating naturally low fructose foods and/or substituting with fructose-free alternatives.
- Eating smaller amounts of excess fructose foods or adjusting portion size to your personal tolerance level
- Using an over-the-counter digestive enzyme called xylose isomerase that converts fructose into glucose molecules for easier digestion.
High Fructose foods (Excess Fructose Foods)
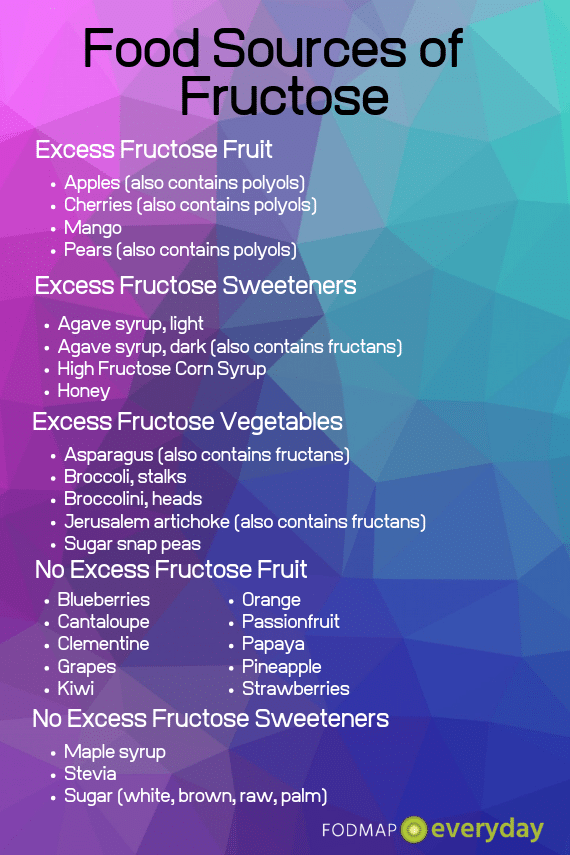
There are a wide variety of foods that naturally contain a high fructose-to-glucose ratio, while others have extra fructose added during the manufacturing process. Common examples include:
- Fruits: Apples, watermelon, cherries, figs, mangoes, pears
- Vegetables: Asparagus, broccolini, sugar snap peas, Jerusalem artichokes
- Sweeteners: Agave nectar, high-fructose corn syrup, honey, molasses
- Beverages: Soda, all fruit juice, apple cider, some sports drinks
- Packaged foods: Breads, crackers, or chips made with high fructose corn syrup; cereal, granola, or snack bars made with honey; dried fruit bars; protein bars sweetened with honey or agave nectar
- Desserts: Baked goods made with honey or with high fructose fruits such as tarts/pies with apple, pear, or fig; sorbet made from high fructose fruits
- Condiments: Jam or jelly made sweetened with fruit juice or high fructose corn syrup, sauces/dressings with honey (e.g. honey mustard), most BBQ sauce, conventional ketchup, hoisin sauce, plum sauce
Low-Fructose Foods
For as many foods that are high in fructose, there are many foods that do not have excess fructose. These foods are likely tolerated by those with DFI, but not necessarily by those with HFI since they do not contain levels of fructose that are low enough to be deemed as safe.
Common examples of low-fructose foods for DFI include:
- Fruits: Bananas, cantaloupe, cranberries, blueberries, oranges, pineapple, lemons, limes, kiwi
- Vegetables: Most vegetables, such as carrots, cucumbers, zucchini, tomatoes, green beans, lettuce, etc.
- Sweeteners: White sugar (aka table sugar), stevia, 100% maple syrup, brown rice syrup, glucose/glucose syrup
- Beverages: Soft drinks sweetened with regular sugar or glucose, lemonade sweetened with sugar, 100% cranberry juice sweetened with sugar, other beverages otherwise sweetened with a low-fructose sweetener
- Packaged foods: Breads, crackers, cereal, granola, snack bars and any other products that are either unsweetened or are sweetened with a low-fructose sweeter
- Desserts: Homemade or commercially baked goods made with table sugar or another approved sweetener, such as Frusano fructose-free desserts.
- Condiments: Jam or jelly made sweetened with sugar only, mustard, soy sauce, vinegars, oil, Heinz organic ketchup, Worcestershire sauce
Dietary management of a hereditary fructose intolerance requires stricter fructose avoidance. While someone with DFI may be able to tolerate fructose in moderation, people with HFI need to keep fructose to a bare minimum(typically less than 1 gram per day).
A strict low-fructose diet involves not only avoiding excess fructose foods as listed above, but avoiding foods that contain sucrose as well. Sucrose is found in table sugar, as well as a variety of sweeteners, fruits, and vegetables. Luckily, those with HFI can still consume most proteins, grains, dairy products, and certain sweeteners.
A variety of fructose-free options are on the market, and products made by Frusano were specifically developed for people with HFI. If you have HFI, working with a specialized dietitian to meet your nutritional needs is recommended.

Be sure to read all about: Frusano The Low Fructose & Low FODMAP Food Company!
The Takeaway
Fructose intolerance is a condition where fructose, a simple sugar and fermentable carbohydrate, is not properly digested and absorbed.
Two forms of fructose intolerance exist – dietary fructose intolerance and hereditary fructose intolerance. Both can be successfully managed through diet, though hereditary fructose intolerance is a more serious condition that requires specialized dietary guidance.
Dietary fructose intolerance can be managed in a similar way to lactose intolerance, including fructose reduction, substitution, and/or enzyme supplementation. Finding fructose-free foods does not have to be a chore! Take advantage of companies like Frusano to make your search easier.
If you suspect you have either HFI or DFI, talk to your healthcare provider about your symptoms and whether testing is appropriate. DFI can be explored with a registered dietitian and low FODMAP diet may be a good starting place.
References
Source #1: Storhaug CL, Fosse SK, Fadnes LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. The Lancet. Gastroenterology & Hepatology. 2017;2(10):738–746.
Source #2: 3. Hadler SL, Locke GR III, Chleck CD, et al. Natural history of functional gastrointestinal disorders: a 12-year longitudinal population-based study. Gastroenterology. 2007;133:799-807.
Source #3 https://pubmed.ncbi.nlm.nih.gov/19403716/
Source #4 https://www.gutnliver.org/journal/view.html?doi=10.5009/gnl20189
Source #5 https://rarediseases.info.nih.gov/diseases/6622/hereditary-fructose-intolerance
This Article Was Generously Sponsored By









Unfortunately I will not be available to attend the Webinar on the schedule date, but I would love to have a copy of the various articles about IBS.
Also I do NOT have a smartphone to download anything that is available about IBS. Is it possible for me to get in PDF format of the various articles/books put out by FODMAP Everyday?
If yes, can you please tell me how much and how do I go about getting these precious articles?
Hi Margaret, all the articles are accessible on our site and are free. Since you posted from the page that the article is on, we know you have already seen it. This article is not in PDF form. We do have some books in PDF form, but you have to download them, so I am not sure what to say. Here is a list of books. If you want to purchase some, we could figure out how to do that and email you the PDFs I suppose, but we cannot do that on an ongoing basis. We could do it in one fell swoop as a courtesy. Look Here.