Many individuals new to the low FODMAP diet wonder why the Elimination phase, where you eliminate all high FODMAP foods for 2 to 6 weeks, is so brief.
After all, if your symptoms are resolving, why on earth would you ever add any of those pain- and gas-producing foods back into your diet? It is tempting (and understandable!) to feel this way.
However, it can have multiple drawbacks for your quality of life and your physical and mental health.
Reasons To Properly Manage A Short Low FODMAP Diet Elimination Phase
Here are some reasons why the Elimination phase is best kept to the recommended timeframe provided by Monash University[1].
Lack of Fiber
The Elimination phase restricts many important sources of fiber that come from fruits, veggies and whole grains. This can lead to constipation, which for many IBS sufferers is either already a problem, or a new problem they just don’t need.
Fiber is also important for overall health: low fiber intake is linked with increased risk of type 2 diabetes, elevated cholesterol, higher risk of cardiovascular disease and possibly and increased risk of colorectal cancer.[2]
Meanwhile, a diet rich in fiber can help with satiety and fullness, leading to better weight control; improved blood sugar regulation; reduced cancer risk; improved immune function and better gut health[3] [4].

Many FODMAP foods are also prebiotics, which serve as a fuel source for our gut bacteria. Without sufficient food, our gut bacteria aren’t able to thrive, and this can change our overall health status and/or impact our ability to digest certain foods.
In addition, taking important fiber “food” away from our gut bacteria means they will sometimes feast on the mucus cells that line our stomach and digestive tract, which can cause a thinning of the epithelial barrier and may lead to inflammation of the gut, or bacteria migrating to places outside our gut.
To learn more about our favorite prebiotic foods read our article Our Favorite Prebiotic Low FODMAP Foods
The science on this is still somewhat nascent, but we are seeing a growing number of links between the gut bacteria, our gut lining and autoimmune disorders.[5] In addition, lack of fiber can lead to other adverse changes in the gut bacteria (“dysbiosis”), such as reduced concentrations of bifidobacteria and butyrate-producing bacteria.
We don’t know yet what the long-term consequences of these changes may be, but initial studies have shown some potential risk for increased IBS symptoms when these bacteria are reduced.[6]
Nutritional Deficiencies
Cutting out multiple food groups for long periods of time can leave you vulnerable to nutritional deficiencies such as B12, folate or iron, which are often found in whole and fortified grains. Fruits and vegetables are rich in vitamins, minerals and antioxidants, however these are often also rich in FODMAPS.
Cutting out too many fruits and veggies for too long can lead to deficiencies in vitamins A, B and C, calcium, iron, potassium, zinc, and of course, fiber. Eliminating dairy products can lead to low intake of calcium, vitamin D and other nutrients.
These deficiencies collectively can lead to increased risk of health problems such as bone loss, anemia, poor healing, electrolyte imbalances, etc.

In addition, those who already follow a restricted or limited diet (vegan, vegetarian, gluten-free) for medical, religious or ethical reasons are now reducing even more foods during the FODMAP Elimination phase. Multiple restrictions can leave you short on protein, iron, fiber and many other nutrients that are required for good health.
Social Isolation
Eating an extremely low FODMAP diet can be very challenging and requires a lot of planning. While the Elimination phase is key to calming gut symptoms so that a structured Challenge phase can identify specific triggers, there is a lot you simply cannot eating during Elimination.
Many typical foods you may have eaten previously are now (temporarily) off limits. Eating in restaurants or out with friends can be very difficult or frustrating. Thus, some people simply stay at home.
This social isolation can lead to or exacerbate depression, which is common in IBS sufferers, so broadening one’s diet during the Challenge phase to the maximum extent possible can help open doors to meals with others without a lot of added stress.
For helpful ideas on how to manage eating out while following the low FODMAP diet see our article Top 10 Strategies for Eating Out On the Low FODMAP Diet

Disordered Eating
Placing a large number of restrictions on one’s dietary intake can cause a great deal of stress. And, if an individual has had painful GI symptoms for years resulting from food intake, it can be very nerve-wracking to eat certain foods, or in some cases, to eat anything at all.
Then, when some individuals enter the Elimination stage, they find they feel so much better they cannot imagine reintroducing foods, because those foods are associated with previous pain.
This is absolutely understandable. However, this also presents a “slippery slope” of sorts where the individual begins avoiding even more foods or adds another diet on top of the FODMAP Elimination phase, and isn’t able to select and follow a well-balanced, nutritionally replete diet.
Recent studies have shown that in patients with celiac disease, IBS, and IBD, rates of disordered eating were between 5% to 44%[7]. These changes in eating habits and aversions to food can, in some cases, lead beyond disordered eating into a full-blown eating disorder if it is not recognized early.
Dietitians are attuned to these signals in their patients and clients and thus will carefully monitor eating habits and intake over the course of several sessions. This is one of the many reasons we recommend working with a trained FODMAPs dietitian.
Please see our articles on Eating Disorders, and also on The Low FODMAP Gentle Diet.
How To Make It Easier To Follow The Elimination Phase
We have written an entire article on how to make it easier to follow the Elimination Phase of the low FODMAP diet! Be sure to check it out here.
The Takeaway
The low FODMAP diet consists of three unique phases: Elimination, Challenge and Integration. Each has specific objectives. Each phase is designed to lead into the next, and is not intended to be a “standalone” or permanent, until you get to the final, maintenance phase.
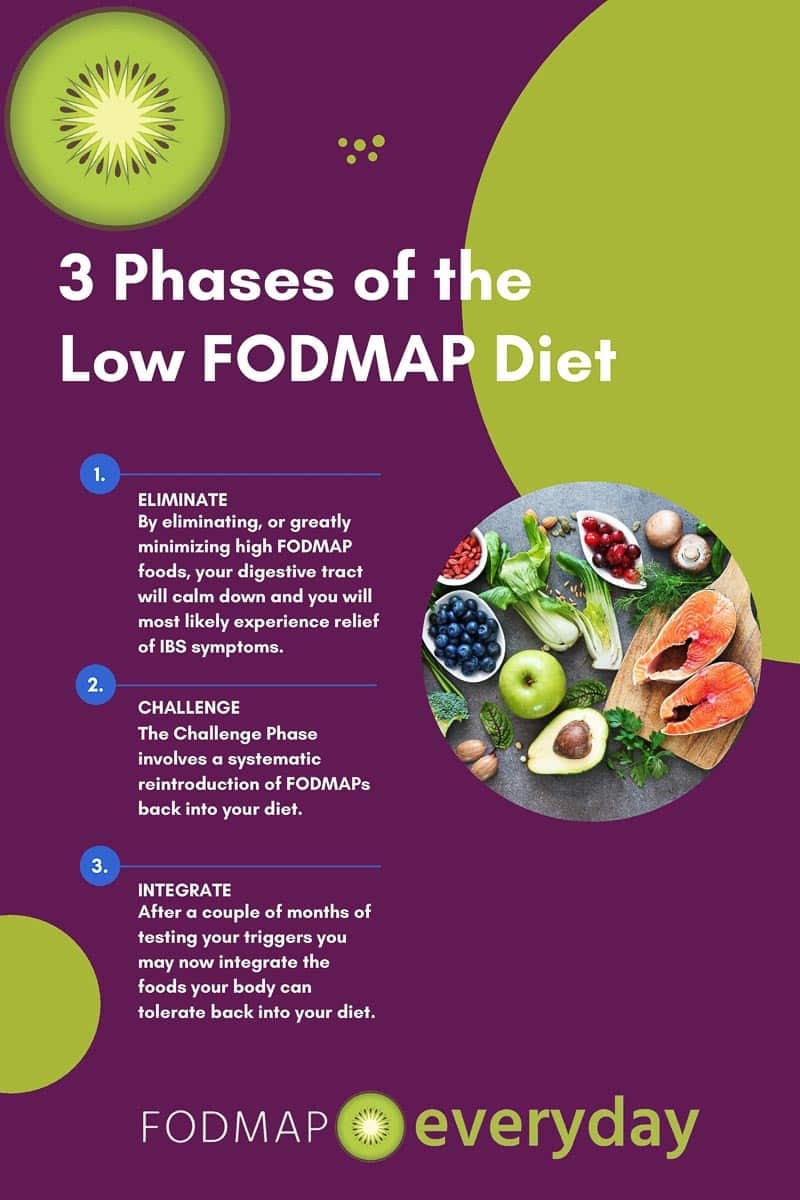
If you are struggling with the transition from Elimination to Challenge or from Challenge to Integration, please seek the help of a trained FODMAPs dietitian. They can help you troubleshoot to ensure you find the right combination of foods that work best for your specific symptoms and nutritional needs.
Use our FODMAP Everyday® RDN Resource Listing Pages to help find dietitians that work with the low FODMAP diet. Always check individual credentials. Some dietitians have completed a course from Monash University, which is an additional level of education that is highly regarded and recommended.
We also have almost 1000 delicious low FODMAP recipes that are appropriate to eat while following the Elimination Phase and beyond – from basics to the sublime. There is no reason for you to feel deprived while making new and healthy choices for your body!
References
[1] The 3 phases of the Low FODMAP diet – Monash Fodmap. Available at: https://www.monashfodmap.com/blog/3-phases-low-fodmap-diet/ (Accessed: 12th April 2018)
[2] Fiber. The Nutrition Source (2016). Available at: https://www.hsph.harvard.edu/nutritionsource/carbohydrates/fiber/. (Accessed: 12th April 2018)
[3] Fiber and Prebiotics: Mechanisms and Health Benefits. (2013). Nutrients, 5(4), pp.1417-1435.
[4] How to add more fiber to your diet. Mayo Clinic (2015). Available at: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983. (Accessed: 12th April 2018)
[5] Hill P, Muir JG, Gibson PR. Controversies and Recent Developments of the Low-FODMAP Diet. Gastroenterology & Hepatology. 2017;13(1):36-45.
[6] Catassi, G., Lionetti, E., Gatti, S. and Catassi, C. (2017). The Low FODMAP Diet: Many Question Marks for a Catchy Acronym. Nutrients, 9(3), p.292.
[7] Hill P, Muir JG, Gibson PR. Controversies and Recent Developments of the Low-FODMAP Diet. Gastroenterology & Hepatology. 2017;13(1):36-45.








Hello. Thank you for this article. What advice would you give if a person reacts on all groups of fodmaps and decides to stick to an almost complete fodmap-low diet? This because fodmaps lead to extreme flatulence and because of that hemorrhoids (and operations).
Kind regards,
Martijn
Hi there. We do not offer direct medical advice but I’ll mention a few things for you to think about. Firstly I would ask you if you have come to these conclusions on your own? I would assume that you have because if you were working with the dietitian you could be asking these questions of them. It is not unusual for people who are not working with a dietitian to get to a place where they feel stuck. You have a much greater chance statistically of succeeding with this diet if you work with a dietitian. In addition, it is not only unhealthy to stay in the Elimination Phase extendedly, but it is also directly cautioned against doing so. It is ultimately not healthy for your microbiome even though in the short term you are feeling better. You mentioned hemorrhoids and operations and it is not unusual for people to have additional medical issues. All this leads me back to what I said in the beginning, which is consulting with the dietitian is going to be your best bet.
I am a full blast celiac. I was diagnosed in 1998 and have followed the diet faithfully as not to get sick. Later on in life I was diagnosed with diverticulitis and have so many pawlips that a am unable to have any colonascipies for many years. Now I have developed IBS and would really like to know what I can eat and what I cannot eat. I am so tired of pain, nausia, and feeling low. Can you please tell me what I cannot eat to satisfy these three diseases?
Hi Lois, I am so sorry you are dealing with so much. First of all, know that you are not alone. About 37% of people with IBS do you have concurrent issues. We do not dispense direct medical advice, but I can tell you that a registered dietitian, or the equivalent in your country, is the exact person who can help you with your situation. I am attaching a link here for our international dietitian’s directory. Please note that many dietitians are now doing remote sessions, so you do not necessarily have to stick close to home. There is light at the end of the tunnel and a way to manage these medical issues, and a dietitian can hold your hand through the process and help you create a complex unique dietary approach and keep triggers at bay.