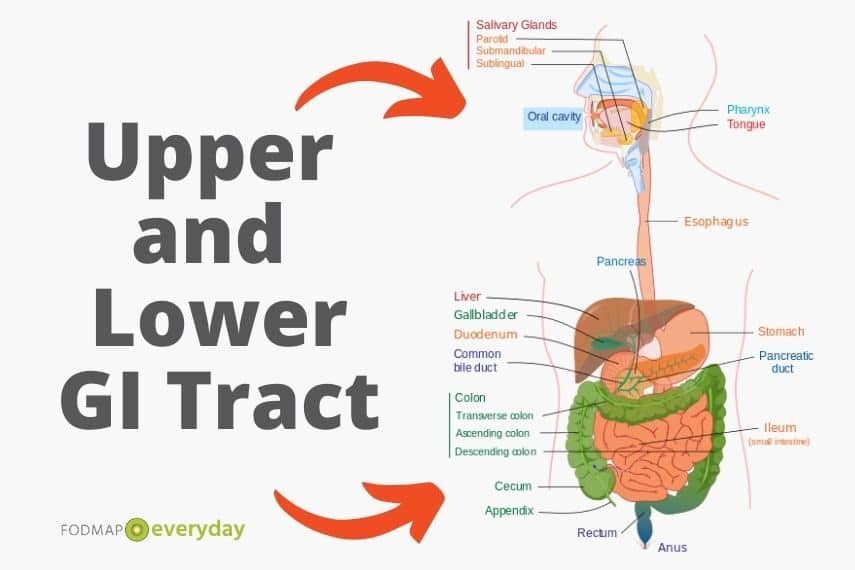
It is common for more than one gastrointestinal (GI) disorder to develop in some individuals, whereby different disorders affect various sections of the GI tract. In some individuals, it may be just the lower GI tract that is affected. For example, an individual may have irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO), or another may have IBS and coexisting celiac disease or inflammatory bowel disease (IBD).
Upper & Lower GI Issues
In other scenarios, both the upper and lower GI tract may develop symptoms, such as individuals who have co-existing IBS and gastroesophageal reflux disease (GERD) or overlapping GERD, IBS and functional dyspepsia (indigestion).
YOU MAY WANT TO READ: SIBO: Get The Facts
Some studies estimate that among individuals with functional GI disorders (FGIDs) – which themselves have an estimated worldwide prevalence of about 20-40% of the population2,3,4 — anywhere between 8-35% have one or more “overlapping” (multiple) FGIDs. 2,3 This combination of gut disorders can increase the complexity of symptom management and reduce quality of life, leaving individuals to struggle with how best to manage myriad nutritional, pharmaceutical and lifestyle interventions.
GERD & IBS
The focus of this article is on the combination of GERD and IBS, as these are the two most frequent upper and lower GI disorders, and they often occur together. The global prevalence of IBS is estimated between 10-15% 5, 6 and the worldwide prevalence of GERD is between 13-25%7, 8.
Definition & Treatment of GERD
GERD is a digestive disorder that affects the lower esophageal sphincter (LES), which is a ring of muscle between the esophagus and the stomach that controls the flow of food and stomach contents.8
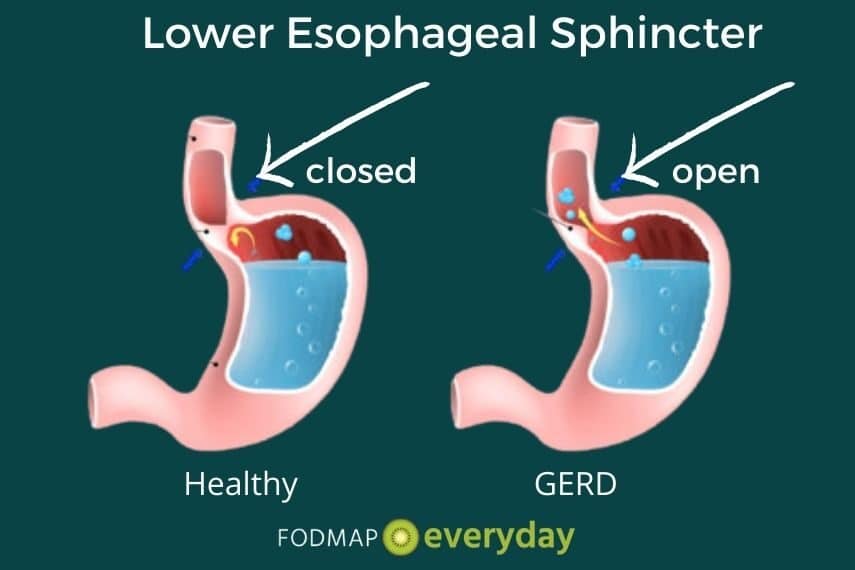
Individuals with GERD suffer from heartburn or acid indigestion caused by stomach acid and partially digested food moving upwards from the stomach into the esophagus instead of downward.
This movement, or reflux, occurs when the LES is weak and/or relaxes inappropriately. The LES can be weakened or influenced by a variety of factors, including certain foods or beverages, smoking, medications, pressure from excess body weight (including pregnancy) or a medical condition called hiatal hernia.8
A hiatal hernia is a condition in which the upper part of your stomach bulges through an opening in your diaphragm. Your diaphragm is the thin muscle that separates your chest from your abdomen. Your diaphragm helps keep acid from coming up into your esophagus.
Most Common GERD Symptoms
The most common symptoms of GERD tend to be burning and discomfort in the stomach and throat, nausea, vomiting, coughing and belching, chest pain, difficulty swallowing and/or laryngitis. Additionally, new or worsening asthma can also be indicative of GERD.
Untreated, GERD can lead to vocal cord or esophageal damage, including Barrett’s esophagus and increased risk of esophageal cancer. Standard treatments for GERD include medications such as antacids, H2 blockers, prokinetics or proton pump inhibitors (PPIs); dietary or lifestyle changes; endoscopic therapy and surgery.9
IBS and GERD Together
While GERD affects the upper GI tract, IBS predominantly affects the lower GI tract, including the small and large intestines. However, the coexistence of the two disorders is where things can get complicated: pressure or symptoms from one area of the GI tract can influence or exacerbate symptoms in the other. For example:
- Lower abdominal gas, bloating and distention, resulting from incomplete digestion and subsequent fermentation of FODMAPs can increase pressure on the stomach and upper GI tract, worsening GERD symptoms such as nausea, belching and heartburn.
- Trapped gas and pressure from chronic constipation or excessive gas production in the small intestine from SIBO may also adversely affect GERD, albeit indirectly.
- Delayed gastric motility (the rate at which food moves through the GI tract) may also simultaneously affect both the upper and low GI tracts, as food languishes in the gut, causing increased IBS and GERD symptoms.
IBS & GERD: Complimentary Dietary Recommendations
| Dietary Recommendations | GERD (7,19) | First-Line IBS Guidance (16,17) | Low FODMAP Diet (18) |
|---|---|---|---|
| Eat a well-balanced diet with a focus on fresh, unprocessed foods. | x | x | x |
| Avoid fried foods and high fat meals | x | x | |
| Avoid spicy foods, tomato products, citrus fruits and foods that may irritate the gut | x | x | |
| Avoid eating large meals | x | x | x |
| Eat slowly and chew carefully | x | x | |
| Reduce your intake of fermentable carbohydrates | x | x | |
| Reduce dairy intake, especially high fat dairy products. | x | x | x |
| Avoid eating right before bed | x | ||
| Try to reduce/manage stress | x | x | x |
| Avoid/limit onions and garlic | x | x | x |
| Avoid excessive amounts of high fiber or gas-producing foods, such as beans or cruciferous vegetables. | x | x | x |
| Limit caffeine, alcohol and/or carbonated beverages. | x | x | |
| Avoid chewing gum or sucking on hard candy. | x | x | |
| Ensure proper hydration and regular physical activity. | x | x | x |
The Low FODMAP Diet and GERD?
We know that the low FODMAP diet (LFD) is an effective treatment for IBS,10,11 but it has not yet been conclusively shown to effectively treat GERD on its own. However, dietary and lifestyle recommendations for GERD often overlap with those for IBS, indicating that there may be some benefit to the LFD for individuals who struggle with both gut disorders.
For example, it is known that gut-irritating foods such as onions, garlic and spicy foods or beverages such as coffee or alcohol can exacerbate symptoms of both GERD and IBS. Lifestyle habits such as exercise, smoking and stress will also affect both disorders in positive or negative ways.
Additionally, some preliminary evidence has shown a connection between certain FODMAPS (fructose and fructans) and inappropriate LES relaxation (leading to reflux of stomach contents), indicating the possibility that reducing the intake of these FODMAPs may help alleviate GERD symptoms.12
There is also a theory that proposes a connection between the treatment of GERD with PPIs (Proton Pump Inhibitors) and the development of SIBO due to decreased stomach acid, which could initiate a cycle of increased gut pressure and gas production, further aggravating GERD symptoms.13, 14, 15
From a clinical perspective, these theories seem to accurately reflect real world scenarios. I, and many of the gut health dietitians I’ve spoken to around the world, have seen substantial success by combining the LFD, GERD dietary recommendations and/or first-line IBS guidance (see box below) as dietary strategies for patients with coexisting IBS and GERD.
Stress, IBS & You
Stress and IBS often co-present. Stress can trigger IBS symptoms, and IBS symptoms can create stress. Read our article on Stress & IBS for ideas on how to alleviate this unfortunate circle.
We have heard from several people in the military dealing with an inordinate amount of stress that exacerbates their IBS. We have an article for you: Dealing With IBS In The Military.
The Takeaway
If you are struggling to manage symptoms for both of these gut disorders, it may benefit you to take a combined approach between the LFD and a GERD diet to maximize overall symptom relief. As always, it’s important to discuss any significant changes to your treatment strategy with your healthcare team – doctor, dietitian, gastroenterologist or other specialist — first.
LOOKING FOR A REGISTERED DIETITIAN?
Be sure to check our Global Registered Dietitian Directory – and remember that many RDNs work remotely as well as in person
References:
- How Long Are Your Intestines? Length of Small and Large Intestines. (2020). Retrieved 3 May 2020, from https://www.healthline.com/health/digestive-health/how-long-are-your-intestines#small-intestines
- Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. The Prevalence and Impact of Overlapping Rome IV-Diagnosed Functional Gastrointestinal Disorders on Somatization, Quality of Life, and Healthcare Utilization: A Cross-Sectional General Population Study in Three Countries. Am J Gastroenterol. 2018;113(1):86‐ doi:10.1038/ajg.2017.421
- Velasco-Benítez CA, Ramírez-Hernández CR, Moreno-Gómez JE, et al. Superposición de desórdenes gastrointestinales funcionales en escolares y adolescentes latinoamericanos [Overlapping of functional gastrointestinal disorders in latinamerican schoolchildren and adolescents]. Rev Chil Pediatr. 2018;89(6):726‐ doi:10.4067/S0370-41062018005000808
- Sperber, A., Bangdiwala, S., Drossman, D., Ghoshal, U., Simren, M., & Tack, J. et al. (2020). Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology. doi: 10.1053/j.gastro.2020.04.014
- Canavan, Caroline et al. “The epidemiology of irritable bowel syndrome.” Clinical epidemiology 6 71-80. 4 Feb. 2014, doi:10.2147/CLEP.S40245
- IBS, U., & Us, C. (2020). What to Do and What to Avoid. Retrieved 3 May 2020, from https://www.aboutibs.org/ibs-diet/ibs-diet-what-to-do-and-what-to-avoid.htm
- World Gastroenterology Organization. (2015). WGO Handbook on Heartburn: A Global Perspective. In World Digestive Health Day. Milwaukee, WI. Retrieved from https://www.worldgastroenterology.org/UserFiles/file/WDHD-2015-handbook-final.pdf
- Information, H., Diseases, D., Adults, A., Facts, D., GERD, D., Center, T., & Health, N. (2020). Definition & Facts for GER & GERD | NIDDK. Retrieved 3 May 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/definition-facts
- Gastroesophageal Reflux Disease (GERD) Treatment. (2020). Retrieved 3 May 2020, from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/gastroesophageal-reflux-disease-gerd-treatment
- Nanayakkara, Wathsala S et al. “Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date.” Clinical and experimental gastroenterology 9 131-42. 17 Jun. 2016, doi:10.2147/CEG.S86798
- Hill, Peta et al. “Controversies and Recent Developments of the Low-FODMAP Diet.” Gastroenterology & hepatology 13,1 (2017): 36-45.
- Geysen H, Gielis E, Deloose E, et al. Acute administration of fructans increases the number of transient lower esophageal sphincter relaxations in healthy volunteers. Neurogastroenterol Motil. 2020;32(1):e13727. doi:10.1111/nmo.13727
- Revaiah PC, Kochhar R, Rana SV, et al. Risk of small intestinal bacterial overgrowth in patients receiving proton pump inhibitors versusproton pump inhibitors plus prokinetics. JGH Open. 2018;2(2):47‐ Published 2018 Apr 2. doi:10.1002/jgh3.12045
- Schmulson MJ, Frati-Munari AC. Bowel symptoms in patients that receive proton pump inhibitors. Results of a multicenter survey in Mexico. Síntomas intestinales en pacientes que reciben inhibidores de bomba de protones (IBP). Resultados de una encuesta multicéntrica en México. Rev Gastroenterol Mex. 2019;84(1):44‐ doi:10.1016/j.rgmx.2018.02.008
- Robillard, N. (2012). Fast tract digestion. Watertown, Massachusetts: Self Health Publishing.
- McKenzie YA, Bowyer RK, Leach H, et al. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016;29(5):549‐ doi:10.1111/jhn.12385
- Cozma-Petruţ, Anamaria et al. “Diet in irritable bowel syndrome: What to recommend, not what to forbid to patients!.” World journal of gastroenterology 23,21 (2017): 3771-3783. doi:10.3748/wjg.v23.i21.3771
- FODMAP food list | Monash FODMAP – Monash Fodmap. (2020). Retrieved 3 May 2020, from https://www.monashfodmap.com/about-fodmap-and-ibs/high-and-low-fodmap-foods/
- Kubo, Ai et al. “Dietary guideline adherence for gastroesophageal reflux disease.” BMC gastroenterology 14 144. 14 Aug. 2014, doi:10.1186/1471-230X-14-144








Really helps… I have GERD andBS.
So glad this was helpful. And while we know you meant “IBS”, we kind of like what you wrote:) Diana is a fantastic RD. Take a look at some of her other articles as well.
I also suffer from Gerd and IBS and I’m looking forward to learn how to manage my life going forward.
It is possible! We highly recommend working with a RD to help you along.
Thank you – very relevant to my conditions
How is this for messed up:
Been on meds for GERD and High Cholesterol for a few years now. Then appendix burst and removed, followed by partial Thyroidectomy (goiter) and gallbladder removed / recently diagnosed lactose intolerance / gluten sensitive – now have IBS (constant diarrhea) and planning my FODMAP diet, hopefully in conjunction with Monash University.
I am so sorry to hear everything that you were going through. I can tell you this, that you are not alone in the fact that you feel that you have a unique complex situation. A great majority of people with IBS are juggling other digestive issues as well. It sounds like you are in very good medical health and we wish you all the luck with what is to come. Are you working with a dietitian?That could be something that could really help you and make the difference
Great article. I’ve had GERD for many years. Since going on the low fodmap diet I seldom have any indigestion and no reflux except if I drink more than one glass of wine. It’s amazing.
Judith what great news! Finding our own individual tolerances is what it’s all about. So glad things are better for you.
I very recently read recommendations that chewing gum can help with GERD, reflux, etc and I find that some gum can. LOTTE Link is the best I’ve found so far but I’m not sure where to buy more. I find a lot of gum flavors unappealing since I just don’t eat things like that.
For decades Finns have chewed xylitol gum to kill streptococcus mutans, the bacteria responsible for dental caries but I read reviewers on Amazon asserting that all sugar alcohols are evil and gum with sugar is effective at cleaning teeth. Xylitol is high FODMAP at something on the order of 70g so I don’t worry about FODMAPs with gum.
Hi Kate, can you link us to the clinical trials where you read this? Would love to see. I have seen some that deal specifically with the esophagus. As far as sensitivity, it varies greatly. EDIT: Our RD responded: “That is a super small study (31 participants) and is not something I’ve ever seen to be recommended by US or global gastroenterological organizations as a therapy for acid reflux. From a FODMAP perspective, gum chewing (esp with artificial sweetened gum) seems to be a dubious recommendation because it can lead to excess bloating (including aerophagia and intestinally-derived) and gas.”
In trying to manage both acid reflux disease (diagnosed over 20 years ago) and IBS-C, I have found that many foods on the low-fodmap list also exacerbate acid reflux. Is there a chart available that can crosswalk foods that work for both conditions?
Thanks!
Hi Shelley, this is exactly what a dietitian can help you with. There is not list, and in fact, the developers of the diet want not to move through the diet if you are also on an other kind of restrictive diet, as this could lead to serious nutritional deficiency. The solution is working with a RD who can tailor a diet to your specific needs.