On September 12, 2020 over 400 clinicians from all over the globe gathered digitally for a “Women In GI Symposium” presented by Epicured, the subscription meal delivery service company that specializes in low FODMAP & gluten-free prepared foods.
The idea was encapsulated by the day’s motto: “Empowered Women, Empower Women”.
The event offered attendees about 5 hours of free educational talks, presented by outstanding women in the GI field, and were able to gain 4.5 Continuing Education Units (CEU) from the Commission on Dietetic Registration (CDR). Epicured tell us that this is the first of what they hope to be many more on-line seminars.
Why Celebrate Women In GI?
As Epicured put forth, although women make up the majority of IBS patients and almost 50% of internal medicine residents, women represent less than 13% of gastroenterologists. To give a voice to the innovative, female thought-leaders in the GI sphere, Epicured wanted to celebrate Women in GI with education and conversation with talks covering topics from the latest in GI health to professional advancement of women in GI.
FODMAP Everyday® Sponsorship & Success Team
FODMAP Everyday® took part as sponsors of the event and also had some of our Success Team RDs (Kathryn Adel MS RD CSSD LD, Diana Reid MPH RD and Rachelle Mallik MA RD LDN), and a visiting RD, Isabel Vasquez of Your Latina Nutrition and a member of Diversify Dietetics, attend specific talks to offer you summaries, which we have included below.
Other sponsors included Sucraid, CDI (Commonwealth Diagnostics International), Schar, Lifeway, Fody, Living Plate, a2 Milk and Beckon Ice Cream.
Agenda & Speakers
Here is a look at the day’s agenda and speakers. Tuck this info away and keep an ear and eye out for future symposiums of similar caliber.
Sign up to be a Partner In Health at Epicured and you will be the first to know about future events as well as have access to a host of other perks.
10:15 – 10:45 am
Elevating the Role of Women in GI: Celebrating Crucial Contributions
Opening Keynote by Amy Oxentenko, MD, FACP, FACG, AGAF
10:45 – 11:15 am
It’s Hard to Tell the Difference: IBS-D vs. SIBO
Judy Nee, MD
11:30 am – 12:00 pm
Understanding the Potential Role of Sucrase-Isomaltase Deficiency and Chronic GI Symptoms
Shanti Eswaran, MD
12:00 – 12:30 pm
IBS-D and Sucrase-Isomaltase Deficiency — Panel Discussion
Panelists: Judy Nee, MD and Shanti Eswaran, MD
12:30 – 1:00 pm
Constipation Remedies
Kate Scarlata, MPH, RDN
1:15 – 1:45 pm
Disordered Eating in GI Conditions
Megan Riehl, PsyD
1:45 – 2:15 pm
Understanding Health at Every Size
Beth Rosen, MS, RD, CDN
2:15 – 2:45 pm
Eating Disorders and Health at Every Size
Moderator: Kate Scarlata, MPH, RDN
Panelists: Megan Riehl, PsyD and Beth Rosen, MS, RD, CDN
2:55 – 3:25 pm
Professional Development Experiences and Opportunities
Moderator: Kate Scarlata, MPH, RDN
Panelists: Aline Charabaty, MD, Megan Riehl, PsyD, Amy Oxentenko, MD, FACP, FACG, AGAF
Summaries & Reviews Of Select Sessions
Below we have summary reviews of:
- It’s Hard To Tell The Difference: IBS-D vs. SIBO
- Understanding the Potential Role of Sucrase-Isomaltase Deficiency and Chronic GI Symptoms
- Disordered Eating In GI Conditions
- Understanding Health at Every Size
- Professional Development Experiences and Opportunities.
It’s Hard to tell the Difference: IBS-D vs. SIBO
Reviewed by Kathryn Adel MS RD CSSD LD
Patients are often confused about SIBO because there is a lot of misleading information all over the Internet, and the symptoms described are very similar to those of IBS-D. Are IBS-D and SIBO different entities, or one of the same? And clinically does it even matter?
Small Intestinal Bacterial Overgrowth (SIBO) is a condition in which bacteria are present in increased numbers resulting in excessive fermentation, inflammation or malabsorption. The prevalence of SIBO is high in IBS patients. According to a study, 78% of IBS patient had positive SIBO breath testing, and after taking antibiotics and eradicating SIBO, they no longer met the Rome criteria for IBS.
SIBO is diagnosed via glucose or lactulose breath test. In practice, most clinicians choose glucose because glucose is more likely to underestimate results whereas lactulose tends to cause false positives. Predictors of a positive breath test are typically biologically female, older age and IBS-D. It is unclear if PPI use is a predictor.
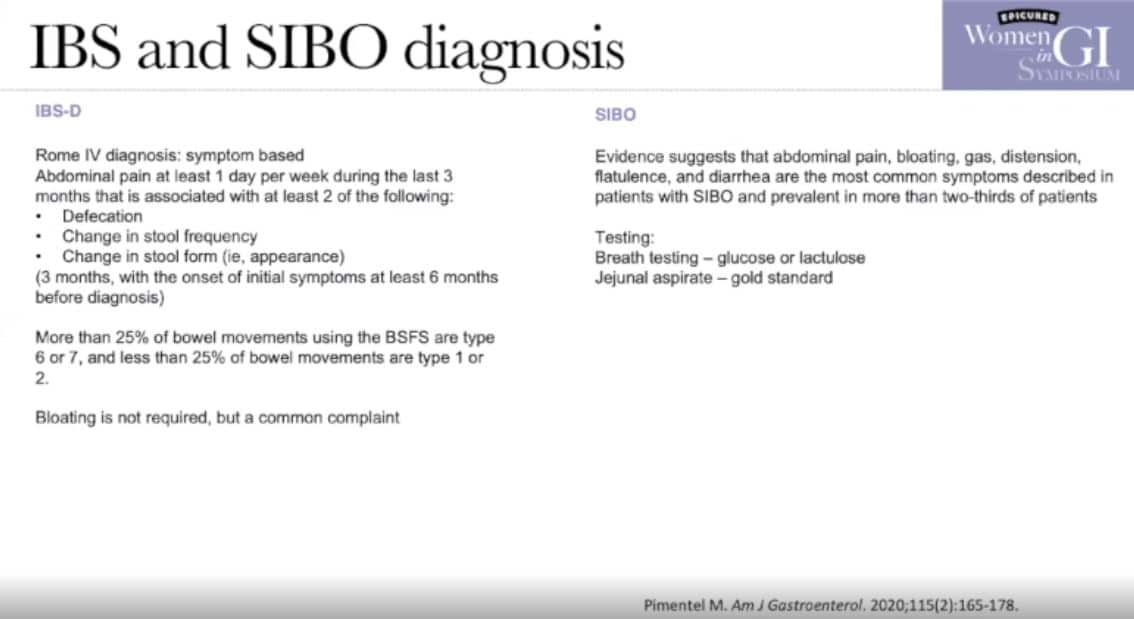
The consensus criteria to diagnose SIBO is greater or equal to 20 ppm hydrogen rise by 90 minutes. However, breath testing for SIBO is flawed and not very reliable. Antibiotics like Rifaximin have been shown to be an effective treatment for IBS-D and SIBO. Small evidence suggests that breath testing can provide an indication on whether antibiotics will help and give a direction on whether or not to prescribe antibiotics.
I was surprised to learn that Rifaximin treatment for IBS-D is becoming more common without SIBO breath testing. As a Registered Dietitian, I tend to want to trial all possible dietary approaches first to try to reduce GI symptoms and avoid the use of antibiotics if possible since they can lead to dysbiosis. The low FODMAP Diet has not been studied in SIBO; this is a good topic for future research.
Takeaways
- Diagnosis criteria for SIBO is flawed, there are false positives and negatives.
- Although there are some guidelines, it remains unclear exactly how to optimally evaluate a patient for SIBO.
- We cannot totally distinguish IBS-D and SIBO, as they can have overlapping diagnoses.
Sucrase-isomaltase Deficiency
Reviewed by Diana Reid, MPH, RDN
The session on sucrase-isomaltase deficiency, and an accompanying Q&A session, was presented by Dr. Shanti Eswaran of University of Michigan at Ann Arbor. Sucrase-isomaltase deficiency (SID) is an often overlooked or underdiagnosed explanation for chronic gastrointestinal distress. In a nutshell, SID is a scenario where an individual lacks sufficient quantities of the digestive enzymes needed to properly digest sucrose (table sugar) and often starches as well.
As background, the body produces a wide variety of digestive enzymes produced by help digest food, breaking it down into very small components, before it can be absorbed into the blood stream and used for fuel. These enzymes include lipase, lactase, palatinase, amylase, trehalase, sucrase-isomaltase, proteases, peptidases, and others.
If the proper enzymes are lacking, absorption of certain foods from the small intestine into the bloodstream does not take place, and the food particles move on to the colon where bacteria there ferment them, causing significant gas, bloating, diarrhea and other uncomfortable symptoms. In the case of FODMAPs, lactose intolerance, due to insufficient lactase production, can be one of the underlying mechanisms for symptoms. But it isn’t always FODMAP sugars that are the most problematic for some people.
Sucrase-isomaltase (SI) is produced in the brush border of the small bowel, and up to 75% of all carbohydrates in the Western diet require digestion via this enzyme. SID is characterized by reduced or complete loss of SI activity. There are two types of SID, congenital and acquired.
The former can be genetically heterozygous or homozygous (one mutation of the SI gene or two), and the latter may be related to compromise of or injury to the small bowel mucosa (the lining of the small intestine) due to issues such as celiac disease, Crohn’s disease, infectious gastroenteritis, or radiation or medication injury. Symptoms can include watery diarrhea, bloating, abdominal pain, unexplained weight loss and/or food aversions and generalized fear of eating. Different mutations can lead to different symptoms or varying degrees of symptom severity. In the past, it was thought that SID only affected children, but this enzyme deficiency is increasingly being recognized in adults.
Diagnosis of SID is done via breath testing (similar to the testing done for SIBO) or a disaccharide assay (which is done using biopsies taken during an endoscopy), with the assay being the “gold standard” diagnostic tool. Treatment is undertaken in conjunction with a registered dietitian and includes a minimum 2-week elimination of sucrose from the diet, followed by gradual reintroduction to assess tolerance levels.
If symptoms remain after this initial no-sucrose trial, dietary starch consumption should also be reduced, as it’s possible that maltase deficiency is also an issue. Utilizing the support of a dietitian is important during this process in order to avoid nutritional deficiencies, as sucrose and starch tend to comprise a very large portion of the typical Western diet.
Finally, there are commercially available enzymes (sacrosidase, or Sucraid) that can help individuals with SID continue to include some sucrose in their diet. This enzyme is not available over the counter and must be prescribed. Typical dosing is about 2cc per meal. Most individuals will find they can increase their sucrose consumption by taking this enzyme, but they still will not be able to eat unlimited quantities.
Takeaways
What is the bottom line? If various dietary strategies have been employed and have not provided sufficient relief from symptoms of IBS-D, and weight loss or malnutrition also seem to be part of your overall picture, talk with your healthcare team about the possibility of SID.
Resources:
- https://www.csiddiseaseinfo.com/
- https://www.csidcares.org/
- https://www.sucroseintolerance.com/symptoms/
- https://www.sucraid.com/
Disordered Eating in GI Conditions
Reviewed by Isabel Vasquez RD
Megan Riehl, PsyD is a GI psychologist who gave the presentation titled, “Disordered Eating in GI Conditions”. As a dietitian passionate about working with clients with disordered eating and eating disorders, this presentation was of special interest to me.
In her presentation, Dr. Riehl discussed the prevalence of disordered eating amongst those with GI conditions. On a worldwide level, the prevalence of disordered eating and eating disorders is on the uptick, occurring at 8.4% in women and 2.2% in men (it is also important to note that men are likely underdiagnosed with eating disorders).
Factors that contribute to the development of eating disorders include genetics, body image distortions, addictions, access to slimming and fad diets, and stress. Notably, many of those with GI disorders related to gut-brain interaction attribute their symptoms to what they eat, piquing their interest in restrictive diets. These restrictive diets can progress to disordered eating and even eating disorders. Having a multidisciplinary team to treat these patients is key and will ideally include a GI doctor, GI dietitian, and GI psychologist who can refer to an eating disorder specialist as necessary.
For individuals with IBS, this presentation displays how important it is to remain conscious of the motives behind eating behaviors. While restricting certain foods may initially be an attempt to manage GI symptoms, it may turn into a desire to control body size and ease body image concerns.
The stress of body image preoccupation can even exacerbate IBS symptoms. There are screening tools available for professionals to assess for disordered eating in their patients, as well as self-screening tools for individuals with IBS to assess their own disordered eating. Note that eating disorders can occur for people at any size and are not limited to those with an underweight BMI.
Takeaways
Dr. Riehl’s presentation reinforced the importance of monitoring overall health by consistently screening for disordered eating in GI patients. Treatments for IBS other than food restriction should be considered for those with disordered eating such as gut-directed hypnotherapy and cognitive behavioral therapy with an eating disorder specialist.
Understanding Health at Every Size
Reviewed by Rachelle Mallik, MA, RD, LDN
I chose to review registered dietitian Beth Rosen’s talk on Health at Every Size (HAES) because it’s an important approach that more providers should be aware of, no matter their area of expertise. I had the pleasure of meeting Beth a few years ago at FNCE (the annual conference from the Academy of Nutrition and Dietetics), and I have attended other webinars where she has been the presenter. She is a wonderful speaker and expert on the topic of HAES and dietary management of gastrointestinal conditions.
At the beginning of her presentation, Beth chose to disclose her privileges (ie. white, cis-gendered, straight- sized body) since they affect someone’s lived experience. I appreciated that this disclosure was relevant to her topic and the symposium at large. She introduced HAES as “a weight neutral approach independent of care.” From my experience, people who are unfamiliar with HAES believe incorrectly that it is healthy at every size, which is not the same as pursuing health no matter what size body you are in. As Beth stated, health is possible independent of weight.
One noteworthy takeaway for providers is that weight stigma is a risk factor for health. Research has shown that a lack of health behaviors or stigma from being a higher weight is more likely to cause health issues than weight or BMI. Beth noted patients she has worked with who have avoided seeing a gastroenterologist for fear of the conversation focusing on weight rather than their GI symptoms.
Advising someone to lose weight and exercise could be harmful. Unless you’ve taken a thorough history of their weight and dieting behaviors, how do you know that the patient has not been on myriad diets, or perhaps they’re currently dieting to lose weight? A patient working with a dietitian could focus on behavior changes rather than weight loss, which is not a behavior. Beth provided examples such as eating smaller meals more often or taking a walk after meals to manage GERD. For someone with IBS, a dietitian can help patients implement the low FODMAP diet (when appropriate) in the least restrictive way to help manage symptoms while maintaining adequate nutrition and nourishment.
An interesting point about dietary restriction came up during the panel discussion on Eating Disorders and Health at Every Size, which was hosted by registered dietitian Kate Scarlata with co-panelist Dr. Megan Riehl, a GI psychologist. Kate and Beth noted a paradox of the low FODMAP diet being less restrictive for some patients. One of the criticisms of the low FODMAP diet is that it can be restrictive, but patients trying to manage GI symptoms or navigate elimination diets on their own may be avoiding even more foods than necessary compared to if they were working with a qualified dietitian.
For those living with IBS, the use of the word “diet” or “dieting” in the context of HAES has to do with manipulating food intake in the pursuit of weight loss. That is different from dietary interventions or medical nutrition therapy to manage diseases or conditions, like a gluten-free diet for celiac disease or the low FODMAP diet for IBS. The low FODMAP diet is not a weight loss diet. Patients may lose weight if they are making significant changes to their eating habits, or they may lose weight due to nutritional inadequacy. This is one of the many reasons people should seek support from a dietitian before trying the low FODMAP diet.
The Takeaway
Beth said she was honored to speak at the Women in GI Symposium because if we help one patient experience less weight bias in healthcare, then we’re making an impact. In a time where language about dieting is shifting away from traditional weight loss approaches to “lifestyle” changes that still promote weight loss and a thin body ideal, Health at Every Size is a refreshing approach backed by research. All healthcare providers can use HAES in their practice to provide weight-inclusive, respectful care to help improve health and well-being. Beth encouraged attendees to take a screenshot of her resources page, which is included below for patients and providers to learn more about HAES.
Resources:
- Health At Every Size, by Linda Bacon, PhD
- Body Respect, by Linda Bacon, PhD and Lucy Aphramor, PhD RD
- Intuitive Eating, by Evelyn Tribole, MS RDN, CEDRD-S and Elyse Resch, MS RDN, CEDRD-S, FAND
- Anti-Diet: Reclaim Your Time, Money, Well-Being and Happiness Through Intuitive Eating, by Christy Harrison, MPH, RD
- Diet Survivor’s Handbook, by Judith Matz, LCSW and Ellen Frankel LCSW
- The Association for Size Diversity and Health (ASDAH)
- Council on Size & Weight Discrimination
- HAES Community
- National Association to Advance Fat Acceptance (NAAFA)
Professional Development Experiences and Opportunities
Reviewed by Isabel Vasquez RD
In the final panel titled “Professional Development Experiences and Opportunities”, Kate Scarlata, MPH, RDN moderated a discussion with panelists Aline Charabaty, MD, Megan Riehl, PsyD, and Amy Oxentenko, MD, FACP, FACG, AGAF.
They were each asked to speak to three things:
1) Their greatest accomplishments and most difficult challenges in their careers
2) A professional advancement tip
3) A tip for being an upstander to uplift other women in the field.
Despite each of their credentials being a bit different, there were certainly common themes throughout all of their responses. Striking a healthy work-life balance was a common response to both their greatest accomplishment and something that has posed a challenge.
In terms of a professional advancement tip, most replied something along the lines of not being afraid to let your voice be heard, pushing yourself outside of your comfort zone, and making room for yourself at the table instead of assuming your voice doesn’t matter.
They all also expressed the importance of uplifting other women through creating community, emphasizing how there is enough space for all of us so the more we support each other, the better off we will be. Another key point made was that you do not have to be at the pinnacle of your career to be an advocate for others. You can do this at any point by speaking up for other women, including them in your projects, and referring to other female practitioners if presented with opportunities you cannot accept.
An interesting consideration about the timing of this panel discussion is the current increase in discussion and recognition around the importance of diversity. While this presentation did allow attendees to hear from a panel of women with amazing professional accomplishments who had great insights for other women in GI, more attention could have been paid to uplifting other underrepresented groups such as racial/ethnic minorities, LGBTQ+ folks, those with disabilities, and those in larger bodies.
Creating communities of women is important, but in order to truly combat the lack of diversity and inclusion, all of these underrepresented groups must also have their voices both listened to and valued. Further research and conversations must include all of these underrepresented groups as well.
A huge THANK YOU to Epicured and all of the sponsors and presenters for conducting such an educational and empowering day.








