In this article we explore the relationship between menopause and IBS. What is menopause, are gut issues affected during this time, and what can be done to help alleviate symptoms?
Definition of Menopause
Biologically, menopause is defined as the point in time when menstrual cycles permanently cease due to the natural depletion of ovarian oocytes (eggs) from aging (1). Practically speaking, menopause is diagnosed after a woman has not had her menstrual period in 12 months.
This usually occurs, on average, at age 50-52 (2), however, there can be wide-ranging differences among women, depending on genetics, race, ethnicity and/or certain lifestyle or environmental factors (such as diet, smoking, alcohol consumption, taking oral contraceptive pills or long-term exposure to endocrine-disrupting chemicals) (2).
While the clinical definition of menopause describes a time after a woman’s menstrual period ceases, it’s the time period prior to medical menopause where women experience the majority of physiological changes and/or uncomfortable symptoms. This is called the menopause transition or perimenopause.
What Happens Physiologically During the Menopause Transition?
The menopause transition can last anywhere from two to five years, and typically, most women don’t notice they are in this phase until they are quite well into it. The overall cascade of biological and physiological changes of the menopause transition is rather complex and consists of many moving parts.
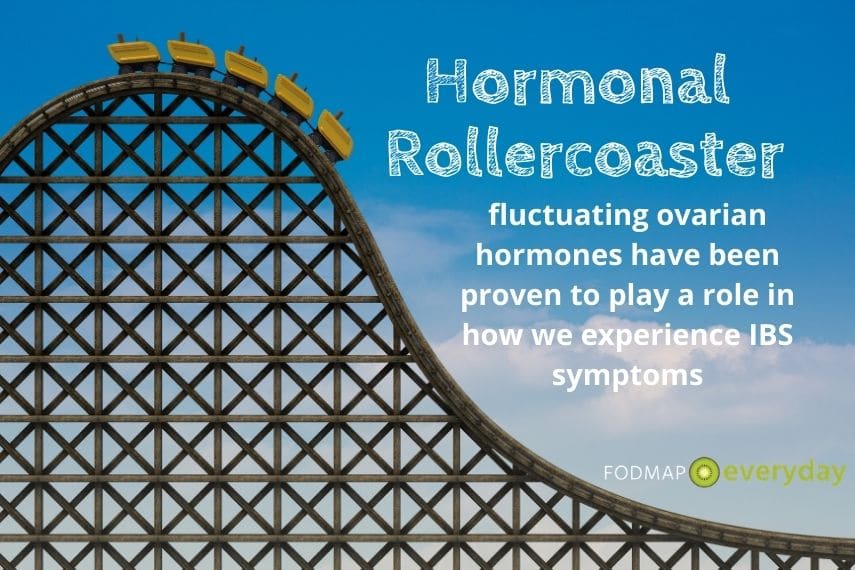
The Hormone Roller Coaster
In a nutshell, during the menopausal transition, the ovaries produce far fewer eggs from increasingly limited follicles, and there are significant fluctuations in reproductive hormone levels (usually an increase followed by a sharp decrease, but this too varies), including inhibin B, follicle stimulating hormone (FSH), estrogen, progesterone and anti-Mullerian hormone (AMH) (2).
These biological changes can then lead to missed or altered menstrual periods and the common symptoms of menopause, such as hot flashes, vaginal dryness, changes to libido, sleep disturbances, mood or mental health disturbances, and weight or body composition alterations. These hormonal shifts can also lead to challenging gut symptoms for many women, as we will discuss next.
Worsening Gut Issues During the Menopausal Transition
It has been long established that irritable bowel syndrome (IBS) symptoms are affected by hormonal fluctuations, particularly changes in a woman’s estrogen and/or progesterone levels. Lower pain tolerance — or a state of visceral hypersensitivity — may also be connected to these same fluctuations.
Thus, many women with IBS have noticed historically that their IBS symptoms become more severe during the premenstrual and early menstruation phases each month (4). And, in fact, many women who do not have a history of IBS or who don’t typically suffer from gut issues in general, may also experience IBS-type symptoms, such as abdominal bloating, pain and/or diarrhea, during these same monthly hormonal fluctuations. This is called dysmenorrhea, or painful menstruation, and it can be truly unpleasant (4).
Hormone Levels Do Affect IBS
As mentioned previously, with the arrival of the menopause transition, our hormones tend to be very volatile – sometimes higher than normal, sometimes gradually declining, and sometimes they take a nosedive and just sort of “crash” for some individuals. Thus, starting in your mid-late 40s, these wide swings in hormonal levels can exacerbate IBS symptoms, whether you are still having a regular menstrual period or not.
One study shows that perimenopausal and postmenopausal women had a high prevalence (i.e. the proportion of women affected out of the total population studied; in this case: 38% vs 14% for premenopausal women) of self-reported altered bowel function, and the prevalence (36%) of IBS-type complaints peaked in the aged 40 to 49 group (6). So, it’s certainly not just a few individuals whose guts are wreaking havoc with the onset of the menopause transition.
In addition, estrogen influences several important pro-inflammatory and anti-inflammatory pathways, and thus, with the significant decrease of estrogen during the menopausal transition, women may be more vulnerable to inflammatory conditions (7). Studies have also shown that gut permeability increases during the menopausal transition and menopausal years, which may trigger inflammation and contribute to gastrointestinal issues among midlife women (8).
You May Want To Read: IBS and Hormones – Information and Strategies
Stress Matters
And of course, it’s been well-documented that gut symptoms are highly correlated to stress (5), and certainly, middle life and menopause prove to be stressful phases of life for many women. Adult children may be heading off to university or otherwise moving away from their nuclear family; paying for these higher education studies can cause significant financial stress for many parents; caring for aging parents can be a challenging task; marriage, relationships and careers often change; and as discussed above, so do women’s bodies (and not always in a way that feels welcome or comfortable). This accumulated stress can disrupt the brain-gut axis, alter gastrointestinal motility, secretion and visceral sensation, and trigger or exacerbate IBS symptoms (7).
You May Want To Read: IBS & Stress: Common Causes and Solutions and The Gut-Brain Connection & IBS: It’s Not All in Your Head article.
Age Matters
Finally, aging itself is also a large elephant in the room. While certain psychological and physiological issues have been directly tied to the menopausal transition, the aging process also lends itself to the development of wide-ranging symptoms such as joint pain or muscle soreness, backache, headache and/or chronic health conditions, such as insulin resistance, osteoporosis, hypertension, or elevated cholesterol levels. Therefore, it can be somewhat challenging to “tease out” the menopausal links from the “just-getting-older” situation and decipher what issue is causing which changes to IBS symptoms.
This All Sounds Super Un-Fun. So What Can You Do?
- It’s important to remember that not every woman with IBS will suffer increased symptoms during this phase of life, however it can be useful to keep the above points in mind as you navigate these new peri- and post-menopausal waters.
- Talk with your doctor, gastroenterologist and/or your gynecologist about ways you can manage your symptoms. It remains unclear if menopausal hormone treatment (MHT) can help reduce menopause transition-induced symptoms of IBS, but it’s certainly worth a conversation to understand what might make sense for your unique health situation and lifestyle.
- Self-care! It’s important to eat well, manage stress and get your nightly 7-8 hours of sleep during this time of life. Try to get plenty of fiber-rich foods (low FODMAP as needed), eat lots of plants, hydrate well, get some daily physical activity, and care for your mental and physical health as best you can. Work with your dietitian if you feel like you could benefit from a “tune up” of your current nutrition plan and eating habits.
- Pro-menopausal resources, such as your local menopause medicine clinic, online support groups, friends and family who are going through the same and/or Dr. Jen Gunter’s fabulous Menopause Manifesto book, can help you better understand all the big changes and reduce some ambiguity or stress. Don’t go it alone!
References:
- Menopause: What is Menopause? Menopause Symptoms, Treatment, Diagnosis – UCLA. Uclahealth.org. https://www.uclahealth.org/obgyn/menopause. Published 2021. Accessed October 26, 2021.
- GUNTER D. MENOPAUSE MANIFESTO. [S.l.]: PIATKUS BOOKS; 2021.
- H.G. Burger, G.E. Hale, D.M. Robertson, L. Dennerstein, A review of hormonal changes during the menopausal transition: focus on findings from the Melbourne Women’s Midlife Health Project, Human Reproduction Update, Volume 13, Issue 6, November/December 2007, Pages 559–565, https://doi.org/10.1093/humupd/dmm020
- Hormones and IBS. UNC Center for Functional GI and Motility Disorders. Med.unc.edu. https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/IBS-and-Hormones.pdf. Published 2021. Accessed October 26, 2021.
- The Role of Gut-Brain Interactions in Influencing Symptoms of Irritable Bowel Syndrome – Gastroenterology & Hepatology. Gastroenterologyandhepatology.net. https://www.gastroenterologyandhepatology.net/archives/january-2018/the-role-of-gut-brain-interactions-in-influencing-symptoms-of-irritable-bowel-syndrome/. Published 2021. Accessed October 26, 2021.
- Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016;150(6):1262–79.e2. https://doi.org/10.1053/j.gastro.2016.02.032.
- Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome?. Gend Med. 2009;6 Suppl 2(Suppl 2):152-167. doi:10.1016/j.genm.2009.03.004
- Yang, PL., Heitkemper, M.M. & Kamp, K.J. Irritable bowel syndrome in midlife women: a narrative review. womens midlife health 7, 4 (2021). https://doi.org/10.1186/s40695-021-00064-5