The Gut-Brain Connection & IBS
Irritable bowel syndrome (IBS) sufferers know all too well the realities of the gut-brain connection: uncomfortable or embarrassing gut symptoms cause stress, which then trigger further painful symptoms.
Or, the reverse is also often true: the fear of encountering symptoms (e.g. when one is planning a vacation or readying for a major life event) leads to the symptoms themselves roaring in. What’s the deal anyway?
This article will explore the gut-brain connection as related to IBS and provide insights for managing this connection to address symptoms and improve your overall quality of life.
- The Gut-Brain Connection & IBS
- The Gut, the Brain and a Trillion Microbes
- Serotonin & IBS Symptoms
- The Gut & The Brain: A Two-Way Street
- How Does Stress Affect the Gut?
- IBS & Hypersensitivity
- It’s Not in Your Head. But Your Brain Plays a Big Role
- Time to See Your Neuro-gastroenterologist or Psycho-gastroenterologist
- Gut-directed Hypnosis Is Gaining Credibility
- How Can You Benefit from this Information?
- More Gut-Brain Resources
- References
The Gut, the Brain and a Trillion Microbes
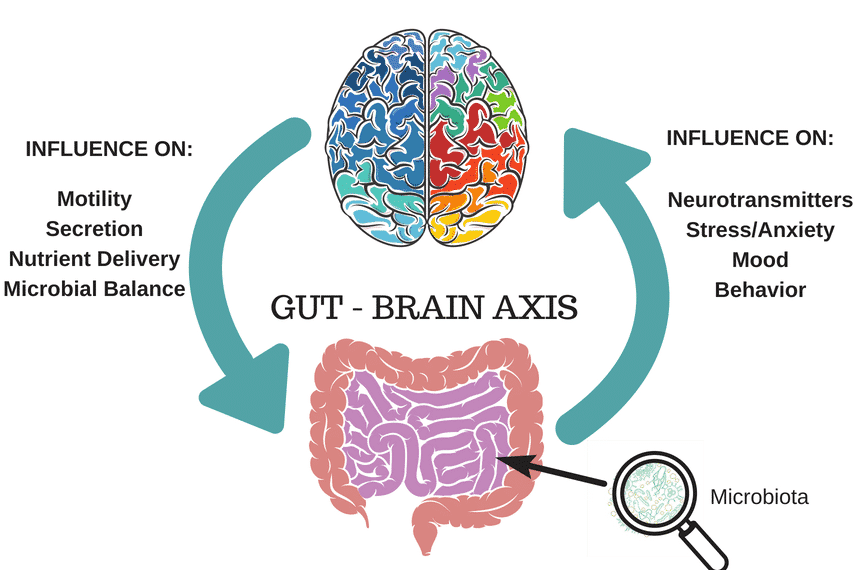
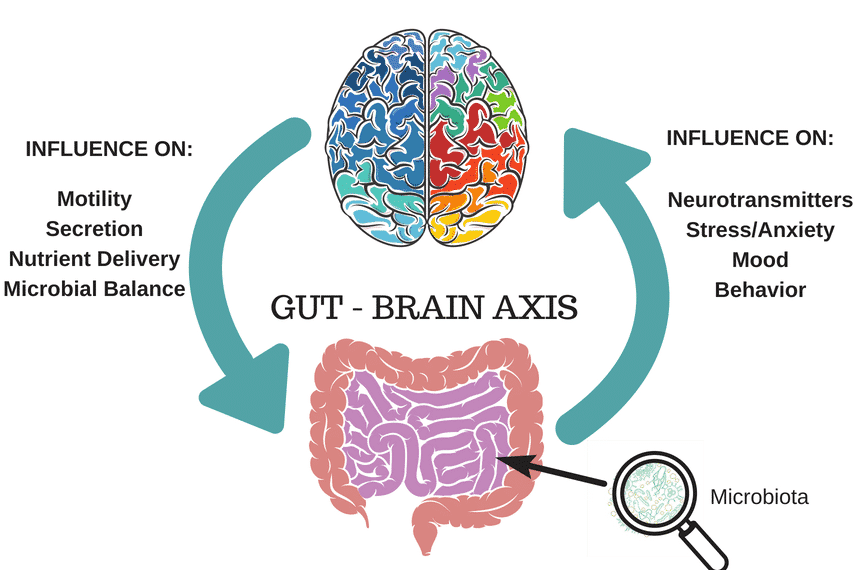
When we think of our nervous system, we often think of the central nervous system (CNS): the brain, spinal cord and related neurons (nerve cells). However, the gut contains as many neurons as the spinal cord!
These more than 200 million neurons, present in the lining of the gut, are part of a network called the enteric nervous system (ENS), or your “gut brain” or “second brain,” which is connected to the CNS via the vagus nerve.
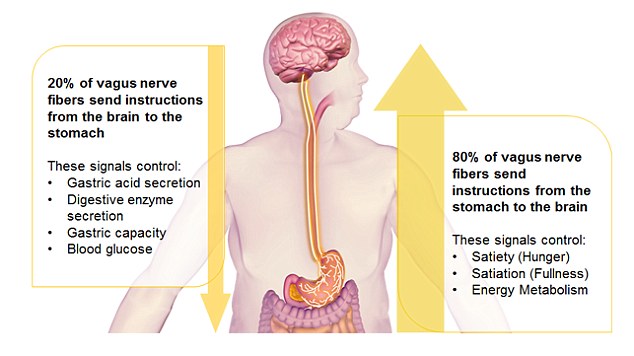
The vagus nerve has a variety of functions throughout the body and plays an important role in stress response, for example slowing our heart rate and breathing. In the gut, the vagus nerve serves to control muscle contraction (peristalsis), secretion of certain substances to aid in GI function and digestion of food, and blood flow to the gut. It also relays important messages from the gut brain to the brain via neurotransmitters, or chemical messengers.
Serotonin & IBS Symptoms
Neurotransmitters, such as serotonin, are produced primarily in the gut with the help of the trillions of microbes that reside there. In fact, it is estimated that more than 90% of the body’s serotonin is produced in the gut, where it plays a major role in communication between the gut and brain.
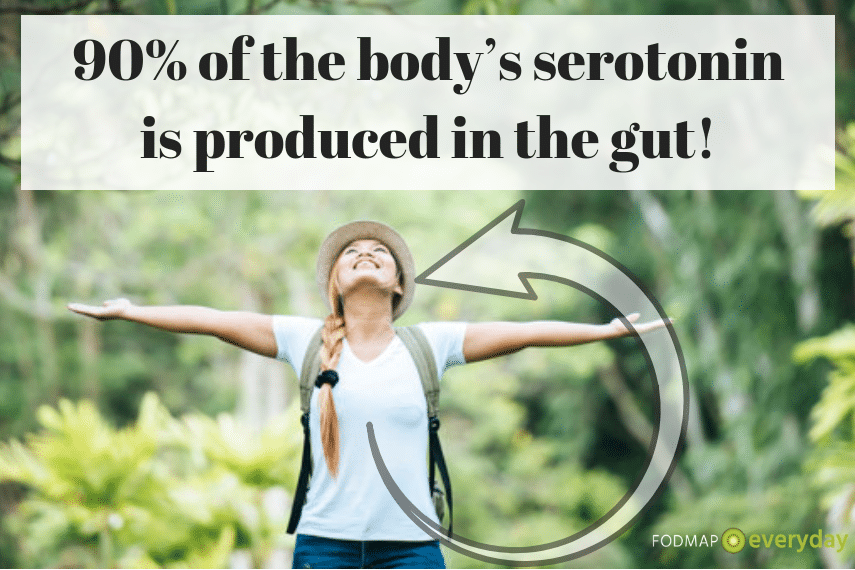
Serotonin (5HT) is one of the most important signaling molecules involved in the peristaltic reflex, which moves food along in our digestive tract, and it’s believed that alterations in serotonin signaling may be responsible for IBS symptoms.
Serotonin is also fondly called the “feel good hormone,” due to its links to mood and feelings of happiness and well-being, which may also help explain the correlation between gut problems and anxiety or mood disorders.
The Gut & The Brain: A Two-Way Street
The role of our gut bacteria is increasingly important as related to the brain and our mental and emotional health. For example, we know that stress can alter the microbial composition of the gut, making it less diverse or more vulnerable to harmful bacteria, which can then lead to increased inflammation, and myriad physical and emotional symptoms.
And, the presence of certain types of gut bacteria can also positively or negatively affect the production of certain brain chemicals (i.e. the aforementioned serotonin example).
Altered gut bacteria (“dysbiosis”) is linked to a variety of brain-related disorders, including depression, anxiety, Parkinson’s disease, autism and more. Thus, the microbe-gut-brain connection is one we want to care for and protect.
How Does Stress Affect the Gut?
Now that we’ve discussed how bacteria inside our guts can affect mental and emotional health, let’s take a closer look at this topic “from the outside in,” and explore how external stressors can affect our gut and its resident microbes.
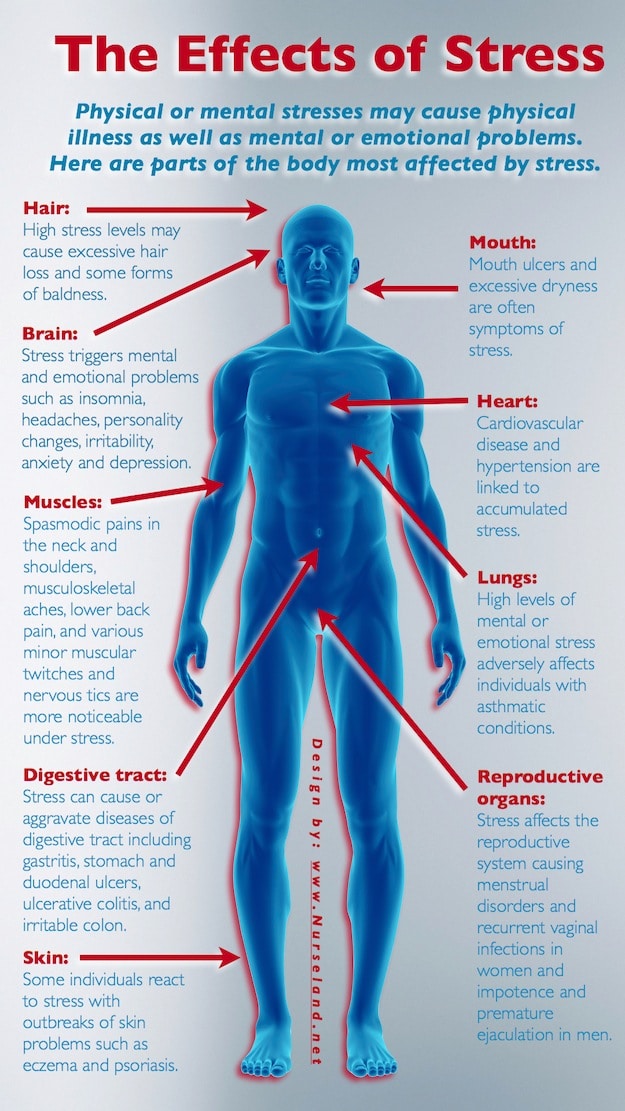
It is well known that IBS is a disorder that is highly correlated with stress. Studies have shown that approximately 60% of IBS patients report the first onset or flare of symptoms in association with psychosocial stressors, such as anxiety, depression, chronic disease, job stress, family concerns or others.
Additionally, IBS patients have a higher rate (10-20%) of diagnosis of an anxiety disorder.
Stress plays an important role in triggering IBS symptoms, as the brain has an increased sensitivity to stressors and responds with reactions or symptoms in the gut.
Stress can affect the movement and contractions of the GI tract by activating specific hormones in the body, such as cortisol, which may divert blood flow from the gut, affecting digestion and overall GI function. Stressors can also affect hasten or slow the movement of the GI tract.
As an example, consider how stress makes your bowels respond when you’re readying for a big presentation or that important 10K race! In addition, stress-based thoughts, feelings and activation of parts of the brain that have to do with anxiety or arousal can stimulate exaggerated gut responses and increase gut sensitivity.
You May Want To Read: IBS & Stress – Common Causes and Solutions
IBS & Hypersensitivity
IBS is characterized by visceral hypersensitivity, whereby the patient has a heightened response to signals of pain that arise from normal physiological reactions, such as gas or abdominal fullness. In short, people with IBS feel pain in their gut more rapidly and more intensely than typical individuals.
This chronic visceral hypersensitivity is shown to involve the brain, resulting in powerful amplification of these sensory signals and continuing the negative feedback loop of increased perceived levels of pain.
So once again, we see a connection between what’s happening between our environment, the gut and what’s ultimately felt or perceived by the brain.
It’s Not in Your Head. But Your Brain Plays a Big Role
Historically, the method of diagnosis for IBS has been one of exclusion, where physicians rule out a variety of other disorders before confirming IBS. This has led to many IBS sufferers feeling unsure about their diagnosis or as if the pain and discomfort must be “all in their head.”
So, one might feel a bit concerned that the idea of a gut-brain connection just adds to this stigma. However, I’d argue just the opposite: Now that we know that the gut and brain are closely inter-related and reflect real world physiological issues, we can better understand IBS and seek to identify innovative new targets for treatment!
Time to See Your Neuro-gastroenterologist or Psycho-gastroenterologist
The relatively new field of neurogastroenterology and the very new field of psychogastroenterology play important roles in this area.
Neurogastroenterology encompasses the study of the brain, gut and their interactions as related to the understanding and management of gut motility and functional GI disorders.
Meanwhile, psychogastroenterology seeks to understand the complex web of links between psychological factors and gut-brain dysregulation.
Researchers and practitioners in these fields continue to explore the gut-brain paradigm in order to identify and advocate for treatment strategies that address all pieces of the puzzle.
Examples of developments in this area include the use of low dose anti-depressants for IBS patients, as they can serve to calm symptoms by acting on nerve cells in the gut.
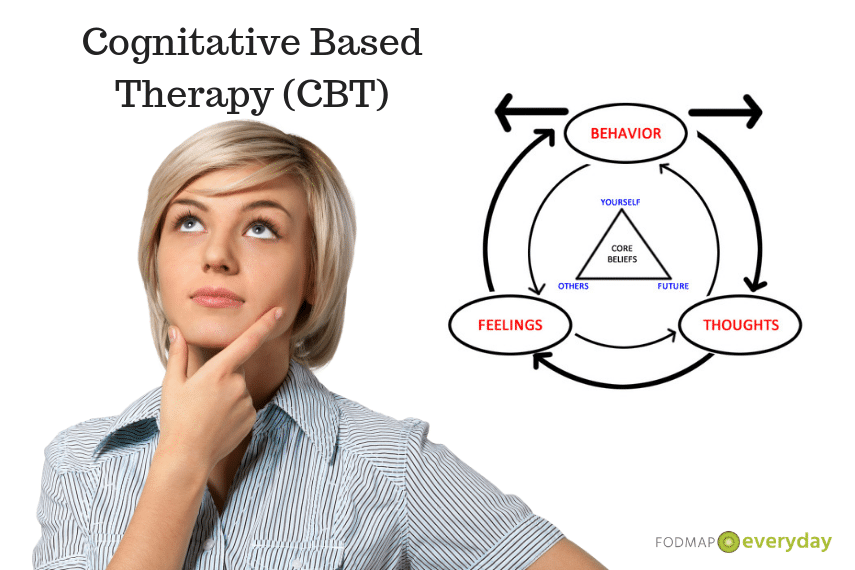
Another treatment strategy is the use of cognitive-based therapy (CBT) or acceptance and commitment therapy (ACT) for the treatment of IBS and related pain management.
Gut-directed Hypnosis Is Gaining Credibility
Gut-directed hypnosis is yet another important treatment that is increasingly backed by scientific evidence for reducing pain and stress associated with IBS.
Psychological therapies work by acting on the frontal or “executive function” areas of the brain to modify cognitive, behavioral and emotional responses to IBS symptoms, which can ultimately help reduce anxiety that results from anticipating or experiencing these symptoms.
And as we discussed earlier, this anxiety, if not checked, can exacerbate IBS symptoms by activating the enteric nervous system, creating that vicious cycle of symptoms of: stress → worsening symptoms → increased stress.
Perhaps the most important activity of the fields of neurogastroenterology and psychogastroenterology is to generate global recognition in the healthcare industry — and beyond — of the gut-brain connection and the interrelatedness of physical, psychosocial and neurological symptoms, thereby validating the patient experience and reducing stigma on behalf of the patient.
How Can You Benefit from this Information?
It’s all well and good to know that our brain and gut are inextricably linked, but what can you do today to help address your IBS symptoms? Here are some suggestions:
- Practice some form of stress relief activity daily, such as yoga (read our Yoga Series here), meditation, diaphragmatic breathing or tai-chi. These practices can help stimulate the vagus nerve and relay soothing messages to the brain and gut.
- Talk to your healthcare provider about the possibility of medication that can target both your mental and physical health, such as low dose SSRIs (anti-depressant medications), serotonin receptor agonists or antagonists. These may help improve serotonin release and uptake.
- Make sure to get sufficient and high-quality sleep. You can find a few tips on improving sleep hygiene here.
- Consult with your physician or mental health professional about other therapies, such as CBT, ACT, talk therapy or gut-directed hypnosis to aid in symptom management.
(Note: You should continue to follow any other treatment strategies, such as medications or dietary modifications as directed by your healthcare team. The strategies mentioned in this article are not intended to be standalone treatments for IBS).
More Gut-Brain Resources
Here are a few more articles and resources to help you in your journey toward feeling better.
- Rome Foundation Psychogastrogenterology Section, https://theromefoundation.org/working-teams-and-committees/rome-psychogastroenterology-committee/
- The Drossman Center, https://drossmancenter.com/education/videos-2/ or https://drossmancenter.com/blog/
- Talking Gut Podcast, https://player.fm/series/talking-gut-with-dr-jim-kantidakis
- The Gut Centre Podcast, https://thegutcentre.com/blog/podcast
- Follow these hashtags on Twitter: #gastropsych, #psychogastroenterology, #GIPsych, or follow doctors Laurie Keefer (@drlauriekeefer), Tiffany Taft (@DrTiffTaft), Megan Riel @DrRiehl or Doug Drossman (@DDrossman).
- Recent articles in the general media:
- Tonic, https://tonic.vice.com/en_us/article/kzxm9m/is-hypnosis-good-for-ibs-symptoms
- Healthline, https://www.healthline.com/health-news/i-tried-hypnosis-to-help-manage-my-ibs-heres-what-happened
- Healio, https://www.healio.com/gastroenterology/irritable-bowel-syndrome/news/print/healio-gastroenterology/%7Bd3ff0190-8631-4157-9b91-a2500081c7ab%7D/gi-psychologists-bring-value-to-ibs-patient-care
- VeryWell Health, https://www.verywellhealth.com/cbt-cognitive-behavioral-therapy-for-ibs-1945355
- Healio, https://www.healio.com/gastroenterology/curbside-consultation/%7B14477a97-aec3-41f6-8515-c7a0ed098293%7D/what-is-the-role-of-ssri
References
- Publishing, Harvard. “The Gut-Brain Connection – Harvard Health”. Harvard Health, 2018, https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection. Accessed 4 Dec 2018.
- “The Role of Gut-Brain Interactions in Influencing Symptoms of Irritable Bowel Syndrome” Gastroenterology & hepatology 14,1 (2018): 44-46.
- Mayer, Emeran A. “Gut feelings: the emerging biology of gut-brain communication” Nature reviews. Neuroscience 12,8 453-66. 13 Jul. 2011, doi:10.1038/nrn3071
- “ANMS – American Neurogastroenterology And Motility Society”. Org, 2018, https://www.motilitysociety.org/. Accessed 4 Dec 2018.
- Diana Swift. “Meta-Analysis: Antidepressants, Psychological Tx Ease IBS”. Com, 2018, https://www.medpagetoday.com/gastroenterology/irritablebowelsyndrome/74981. Accessed 4 Dec 2018.
- “Antidepressants, Psychological Therapies Reduce IBS Symptoms”. Com, 2018, https://www.healio.com/gastroenterology/irritable-bowel-syndrome/news/online/%7Bf84b2280-f93e-465b-b906-55fe250f3026%7D/antidepressants-psychological-therapies-reduce-ibs-symptoms. Accessed 4 Dec 2018.
- Harding, Kaitlin et al. “Reduced Symptoms of Post-Traumatic Stress Disorder and Irritable Bowel Syndrome Following Mindfulness-Based Stress Reduction Among Veterans”. The Journal Of Alternative and Complementary Medicine, 2018. Mary Ann Liebert Inc, doi:10.1089/acm.2018.0135. Accessed 4 Dec 2018.
- “IBS And Serotonin | Gastrointestinal Society”. Gastrointestinal Society, 2018, https://www.badgut.org/information-centre/a-z-digestive-topics/ibs-and-serotonin/. Accessed 4 Dec 2018.
- Predictors Of Outcome In Cognitive And Behavioural Interventions For Irritable Bowel Syndrome. A Meta-Analysis. 2018. Accessed 5 Dec 2018.
- “Gut Directed Hypnotherapy For IBS – Hypnosis To Treat IBS | Michigan Medicine”. Uofmhealth.Org, 2018, https://healthblog.uofmhealth.org/digestive-health/gut-directed-hypnotherapy-ibs-ibd-gerd. Accessed 4 Dec 2018.
- Peters, S. L. et al. “Review Article: Gut-Directed Hypnotherapy In The Management Of Irritable Bowel Syndrome And Inflammatory Bowel Disease”. Alimentary Pharmacology & Therapeutics, vol 41, no. 11, 2015, pp. 1104-1115. Wiley, doi:10.1111/apt.13202. Accessed 4 Dec 2018.
- Keefer, Laurie et al. “Best Practice Update: Incorporating Psychogastroenterology Into Management Of Digestive Disorders”. Gastroenterology, vol 154, no. 5, 2018, pp. 1249-1257. Elsevier BV, doi:10.1053/j.gastro.2018.01.045. Accessed 5 Dec 2018.







This is very detailed and informative! There’s actually evidence that keeping your stress under control can help you prevent or ease IBS symptoms. Through the use of relaxation exercises, you can turn off the stress response, in which gut changes come about in response to thoughts and feelings.
Yes, all very true! The gut and the brain generally work in concert together in a positive way, but when one of them gets out of sync it’s important to try to bring them back together. Relaxation exercises, meditation and other things such as yoga are all great strategies.