It Is Common For IBD & IBS to Co-Exist
One of the happiest days in the life of someone with inflammatory bowel disease (IBD) should be when they get the good news that their disease is in remission. But, this isn’t how it plays out for everyone.
Lots of folks continue to experience intestinal symptoms despite their inactive disease. That’s because up to 40% of people with IBD also suffer from irritable bowel syndrome (IBS). It is not uncommon for IBD and IBS to co-exist. These people have a poorer quality of life compared to those with only IBD.
So, you may ask: What if I have IBS and IBD at the same time?
Fortunately, dietary and lifestyle modifications can significantly improve IBS-related symptoms in people with IBD in remission.
The Low FODMAP Diet Can Help
In this article, I will explain how I use the low FODMAP diet to help these patients.
- The low FODMAP diet is a clinically proven diet to help up to 75% of those with IBS.
- The low FODMAP diet has been shown to improve ongoing symptoms in at least 50% of IBD patients in remission.
But, first, let’s review IBD and how it compares to IBS.
What Is Inflammatory Bowel Disease?
IBD is a chronic, systemic, relapsing, immune-mediated inflammation of the intestinal tract. Over 3 million people in the United States have IBD with varying levels of severity.
We don’t know what causes it, but researchers suspect a combination of genetics and environmental factors are at play.
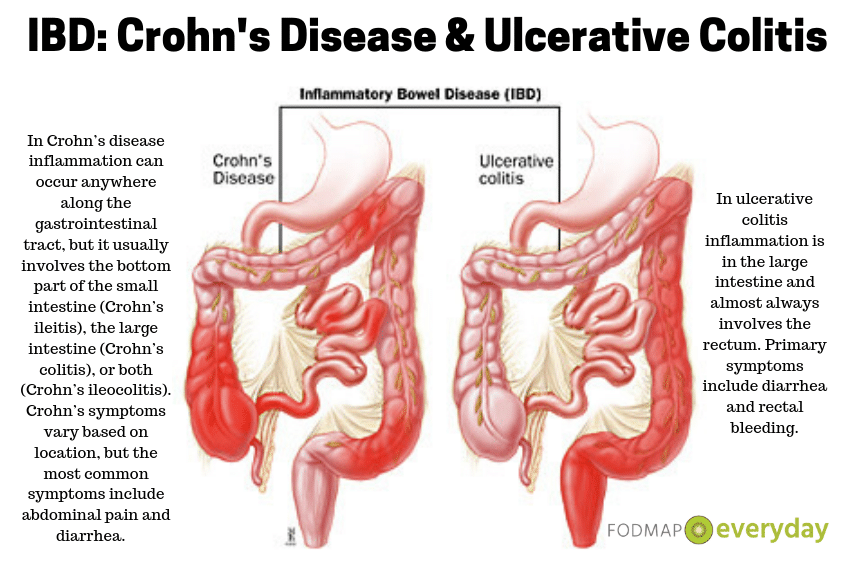
The two main types of IBD are Crohn’s disease and ulcerative colitis.
In ulcerative colitis inflammation is in the large intestine and almost always involves the rectum. Primary symptoms include diarrhea and rectal bleeding.
In Crohn’s disease inflammation can occur anywhere along the gastrointestinal tract, but it usually involves the bottom part of the small intestine (Crohn’s ileitis), the large intestine (Crohn’s colitis), or both (Crohn’s ileocolitis). Crohn’s symptoms vary based on location, but the most common symptoms include abdominal pain and diarrhea.
Both Crohn’s and ulcerative colitis can lead to extraintestinal (out of the intestines)l complications, such as inflammation of the joints, skin and eyes.
Most people with IBD rely on medications to achieve and maintain remission. Some require surgery, including bowel resections and/or colectomy. Severe cases of IBD can lead to life-threatening complications, including colon cancer.
Key Similarities & Differences Between IBD & IBS
IBS is a brain-gut disorder usually involving the small and large intestines with disturbances of gut motility and sensation. Affecting approximately 45 million Americans, it is the most common functional gastrointestinal disorder.
YOU MAY WANT TO READ: The Gut-Brain Connection & IBS: It’s Not All In Your Head
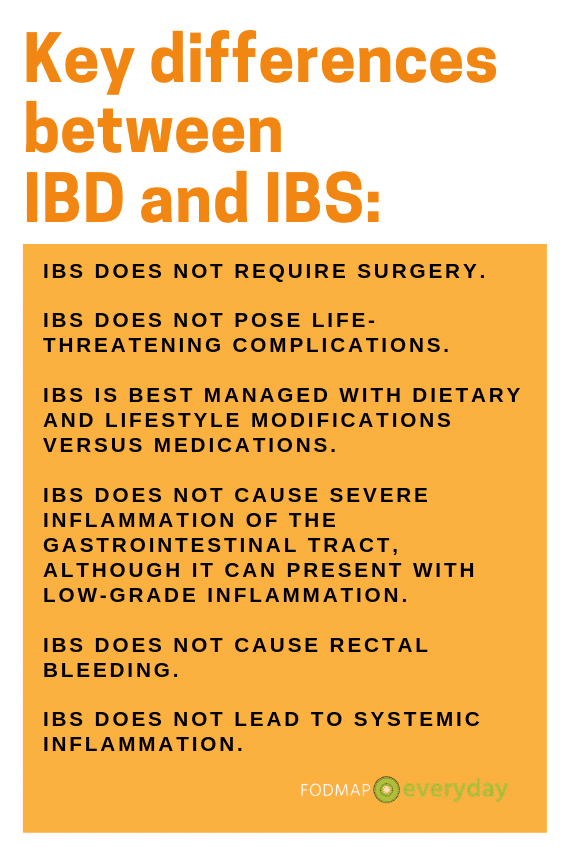
Key differences between IBD and IBS:
- IBS does not require surgery.
- IBS does not pose life-threatening complications.
- IBS is best managed with dietary and lifestyle modifications versus medications.
- IBS does not cause severe inflammation of the gastrointestinal tract, although it can present with low-grade inflammation.
- IBS does not cause rectal bleeding.
- IBS does not lead to systemic inflammation.
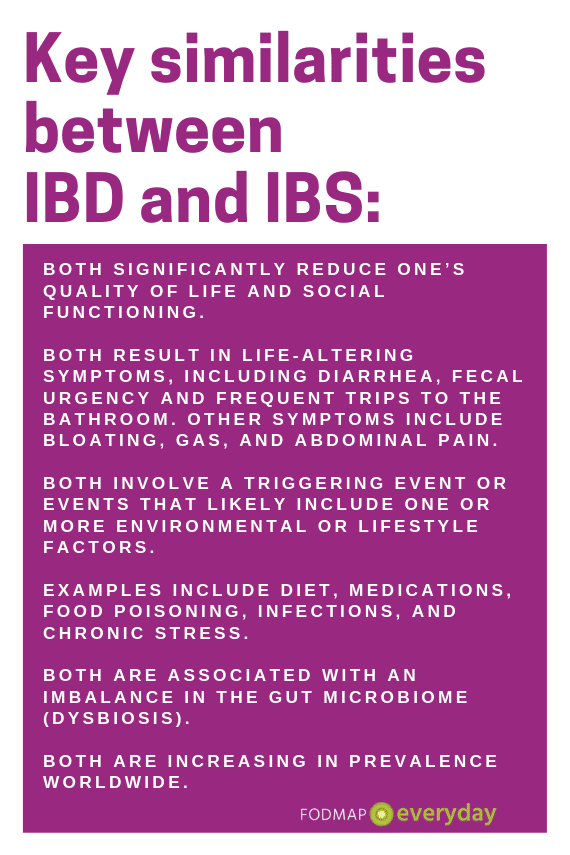
Key similarities between IBD and IBS:
- Both significantly reduce one’s quality of life and social functioning.
- Both result in life-altering symptoms, including diarrhea, fecal urgency and frequent trips to the bathroom. Other symptoms include bloating, gas, and abdominal pain.
- Both involve a triggering event or events that likely include one or more environmental or lifestyle factors. Examples include diet, medications, food poisoning, infections, and chronic stress.
- Both are associated with an imbalance in the gut microbiome (dysbiosis).
- Both are increasing in prevalence worldwide.
Since these conditions have a lot in common, it can be difficult for gastroenterologists to determine if someone’s symptoms are due to IBS or IBD.
Tests Can help Distinguish Between IBS & IBD
Doctors might use one or more of the following tests to differentiate between IBS and IBD:
- Blood work for infection, anemia and/or inflammation.
- Colonoscopy with biopsy.
- Fecal calprotectin, a specific marker of intestinal inflammation.
- Imaging, such as CT or MR Enterography.
The Low FODMAP Diet for IBD
Over the last decade I’ve counseled countless patients with IBD on what to eat. Many people see me because they continue to have symptoms despite being in remission. They need help to identify the food triggers for their overlapping IBS.
Emerging research supports using the low FODMAP diet for managing IBS-related symptoms in patients with inactive IBD, particularly for abdominal pain, bloating and gas. My clinical experience aligns with these findings.
WARNING: Patients and healthcare professionals must be cautious when using any kind of restrictive diet with this population. Nutrient deficiencies, food intolerances, and disordered eating behaviors are common among IBD patients. We must not impose unnecessary dietary restrictions.
If someone can’t do the entire low FODMAP diet, then start with just one or two groups of FODMAPs to eliminate. A registered dietitian can review one’s current diet to help decide where to begin.
Lactose intolerance is more common in people with Crohn’s and ulcerative colitis, and Crohn’s patients are less likely to absorb fructose compared to the general population. Perhaps start by eliminating lactose and/or fructose?
Fiber & IBD
Lots of patients with active and inactive IBD limit or avoid high-fiber foods. Dietary fiber can worsen IBD symptoms. Specifically, high-roughage foods can irritate the bowel causing abdominal pain, bloating, diarrhea, urgency, and bowel obstructions in at-risk individuals. High-roughage foods include raw vegetables, whole nuts and seeds, whole grains, popcorn, and thick skins of fruits and vegetables.
Some people with inactive IBD avoid high-fiber foods out of necessity, others out of fear. Either way, many continue to feel unwell on a low-fiber diet. In lots of cases, these ongoing IBS-symptoms are because of FODMAPs.
Eat Roughage, But Go Low
I’ll recommend a low-roughage, low-FODMAP trial for 2-3 weeks. On this diet patients eat lots of low-FODMAP smoothies, white rice, soups, cooked vegetables, peeled fruit, creamy nut butters, and lean protein.
Frequently when it’s time to reintroduce or challenge foods, I’ll start with higher fiber, low FODMAP foods. Most of my patients are itching to eat more fruits and vegetables, so maybe we’ll start with a few lettuce leaves, a few carrot slices, edamame or grapes.
When these go well, they’re surprised and glad to learn that they don’t have to avoid fiber after all! From there we’ll start challenging FODMAPs. I always recommend a cautious challenge with IBD patients.
Conclusions & Key Takeaways
Up to 40% of people with IBD suffer from irritable bowel syndrome (IBS). The low FODMAP diet can improve IBS-symptoms and quality of life in these patients.
Patients and practitioners must exercise caution when using any kind of restrictive diet with people with IBD because they are at a higher risk for nutrient deficiencies and disordered eating as compared to the general population.
Everyone on a low FODMAP diet should consult with a knowledgeable dietitian.
One of the happiest days in the life of someone with IBD should be when they get the good news that their disease is in remission. The low FODMAP diet might be the missing link in making this a reality for IBD patients with overlapping IBS.







This is very true. However my diet is even more restrictive than lo fo as I also do low fat, low sugar and low caffeine. And if i go over a little but with any variables then I get into trouble. That’s when I go back on ensure plus for few days or week or 2 till symptoms settle down. Then the process begins again. Doesn’t help that even safe lo fo gods don’t agree with me either. Ok
Doesn’t help I also have comorbid functional dyspepsia and GORD. Of course all these are severe. So managing doo many illnesses at once is like a ticking time bomb. Too m ugh of anything is gonna set somethj g else off i can guarantee u. Lots of hard work but I’m worth it. Better than daily pain.
Diana, I love how you ended your comment. You ARE worth it! And I can empathize about the pain. For me, my diet is relatively “easy” in the sense that I KNOW I never want to be in that kind of pain again. Sure, it does get frustrating at times, but that pain memory can help motivate! Do you have a RD or other medical professional that helps you navigate all your needs? This is so much for a lay-person to tackle on their own.
I never had an issue until after I was treated for stage 3 colorectal cancer. After radiation,surgery And chemo my guy went crazy. It’s only gotten worse and it’s been ten years since treatment ended. My gut has never calmed down. It was almost easier when I had my ileostomy while in treatment!
Cindy, you are not alone. It is not unusual for surgical procedures and/or meds to bring on a change. I am so sorry that you are going through this. Do you have a RD to work with?
Would like to follow this group. Had coeliac diagnosed way too late in life. Now have everything else to add to it after so much damage done. Had partial colon removed and some damaged ‘tubing’. Now researching for help with pain bloating and all the rest. Hopefully i will learn something to add to 17 years of research. Thanks
Hi Linda, I am so sorry to hear of what you are dealing with but thankful you have found us. Colleen specializes in IBD and where IBS intersects in particular. We will be having more content created by her with this focus and we also encourage you to reach out to her directly.
Great article. Does the above apply to lymphocytic colitis as well?
Hi Susan,
Thx for your question! A low-roughage, low-FODMAP diet can reduce common symptoms associated with lymphocytic colitis, including bloating, diarrhea and bowel urgency. I strongly encourage anyone considering this approach to work with a knowledgeable RD to determine if you’re a good candidate, get help to reintroduce foods after the elimination phase, consider other potential food and/or lifestyle triggers, and ensure you’re meeting your nutritional needs.
Let me know if you have other questions!
I found that certain foods like popcorn cause me imediate pain and bloating within half an hour. Is this a certain type of food group and if so what other things should I avoid please?
Hi Tracey, we do not offer individual medical advice, but there are a few things to think about. You might find our article in the TIMING of symptoms to be helpful. Also, it would make sense to consult with a medical doctor like a gastroenterologist to assess your digestive issues. You could be screened for diverticulitis, for instance.
Hi,
I am suffering from UC for past 10 years.
I am on Xeljianz, mesacol enemas and suppository for the same. Untill recently I was doing good. But suddenly I have started to have pencil size stool, constipation, suddenly diarrehea (complete watery) but no bleeding or any other discomfort which I get with UC.
I am bit confused what it could be. Please help as I am afraid this episode can trigger my UC.
Hello Akshita, I have reached out to Colleen who can respond when she can. In general we do not give direct medical advice and your situation sounds like communicating with your medical team would be prudent and also get you the quickest answers. We do understand the frustration. Don’t delay in contacting your doctor’s office.
Hi Akshita, I’m sorry you’re not feeling well. To echo Dede, it’s important to work with your medical team to identify the cause of your symptoms so they can treat you appropriately. Lots of things can lead to changes in BMs, such as dietary changes (more/less fiber), fluids (it’s been HOT recently!), less/more activity, stress, etc. I know how scary these changes can feel, especially when you have IBD, but they’re not always cause for alarm. That’s why it’s so important to speak with your clinicians. Also, for what it’s worth, symptoms shouldn’t trigger flares, so maybe that’ll put you at ease a bit? I hope you feel better soon!