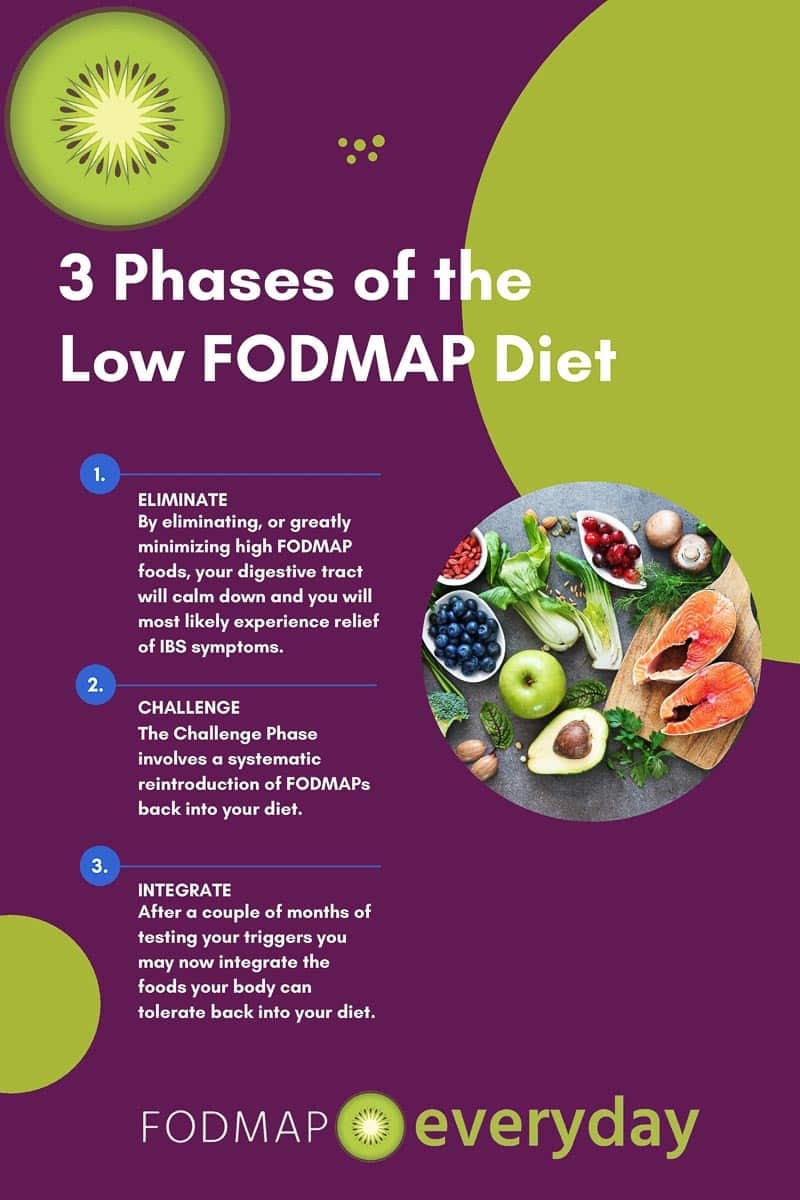
The low FODMAP diet is a THREE-phase diet comprised of Elimination, Challenge and Integration. After many weeks of eliminating foods and the nail-biting (or gut-clenching) process of systematically reintroducing FODMAPs one by one during your Challenge Phase (sometimes called Reintroduction), you’re now ready for Phase 3: The Integration Phase (sometimes called Personalization)!
This article is for those of you who have completed structured Elimination and Challenge Phases.
While you might be ready to jump with both feet into eating all those foods you love and have missed over the past few months, I’m going to advise you to wade in a bit more slowly. (Don’t worry, you’ll still be able to enjoy plenty of food options over time). But, in order to not over-stress your gut, and to continue to carefully monitor any potential triggers, it’s important to undertake Phase 3 in a somewhat structured manner. Here are my key tips.
Organize the Results of Your FODMAP Challenges.
Look back at your Challenge Journal and try to rate your any symptoms experienced during each challenge as none, mild, moderate, or severe. Remember, your level of comfort is very personal, and you get to decide what feels acceptable and what does not.
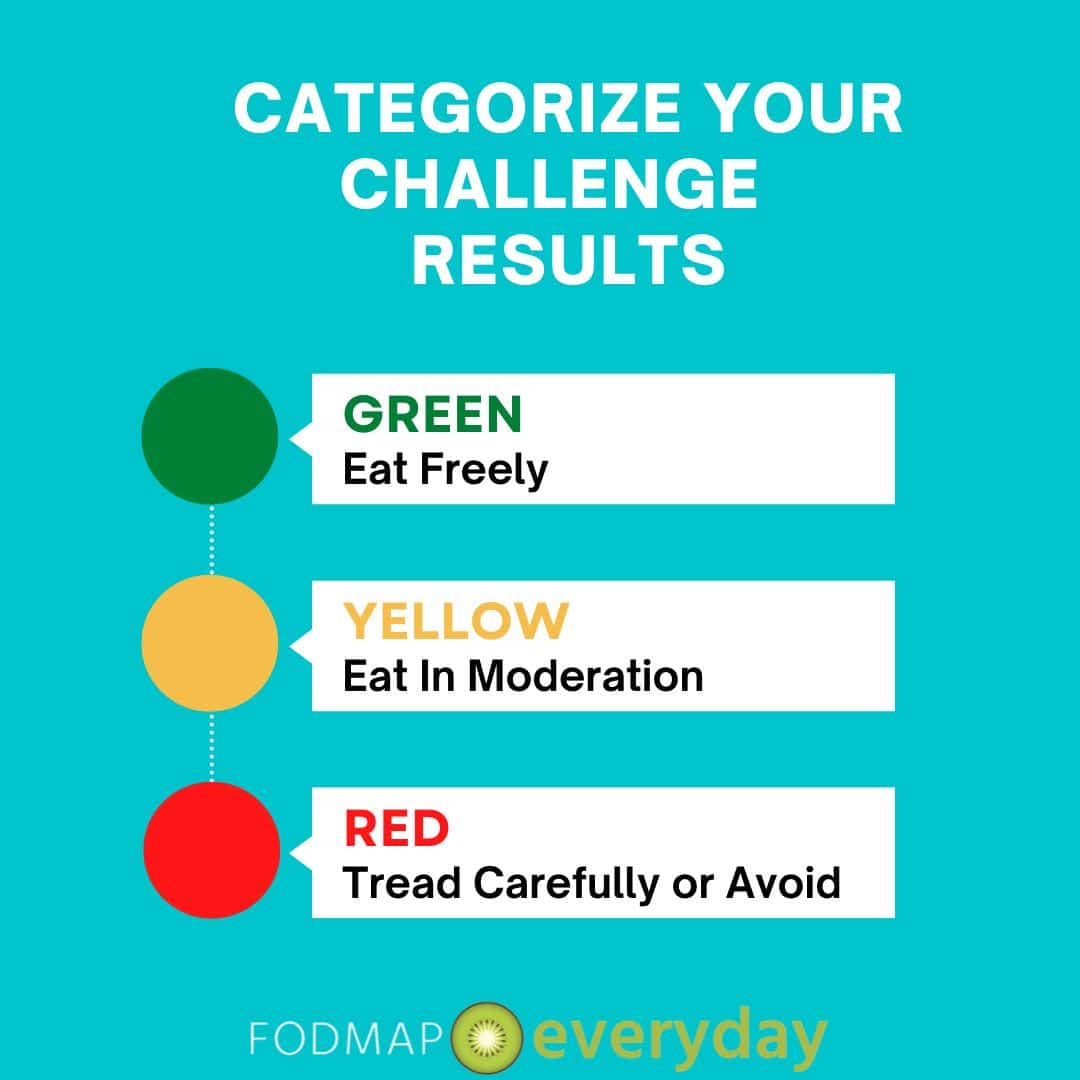
Now, categorize your Challenge Results according to the below:
- Foods you tolerated with mild or no symptoms (well tolerated = Green Foods). These are the foods where you were able to successfully eat the challenge food on all 3 Challenge Days and experienced very little or no effects.
- Foods you found problematic in a moderate or large dose (moderately tolerated = Yellow Foods). For example, perhaps Day 1 of this food brought no symptoms, Day 2 symptoms were mild and Day 3 a bit more moderate.
- Foods where even a small amount was problematic and caused severe symptoms (poorly tolerated = Red Foods). Most likely, Day 1 produced symptoms and you did not complete further challenges of this food.
Once you’ve made your lists, you now have a roadmap to proceed with gradually re-integrating some foods back into your diet. We’ll use the table below to discuss specifically how to approach each group of foods.
Reintroduce Well Tolerated into Your Daily Routine
Let’s begin by reintroducing a small-to-moderate serving of one or more FODMAP-containing foods that you tolerated well into your daily diet for a couple weeks. During this time, continue to monitor any changes in your gut as well as any external factors (such as stress, hormones, travel) that can affect digestion.
Tolerances can be tricky, especially with foods that contain multiple FODMAPs or when eating multiple FODMAP-containing foods in the same meal, so take your time and enjoy the increasing variety of foods. Over time, you should be able to eat most any serving size of your well-tolerated foods on a regular basis.
Reintroduce Moderately Tolerated Foods
After a few weeks of well-tolerated foods, you can now begin to tackle adding back in some of the foods that you enjoy but which caused some mild to moderate symptoms in larger amounts during the Challenge Phase. Pick a few of your moderately tolerated foods and add a serving to your diet every few days to start. (Try not to add multiple serves to the same day or the same meal just yet).
Remember, our goal is the most diverse and nutritious diet possible, so skipping these foods will likely leave your nutritional intake overly limited.
Remember, our goal is the most diverse and nutritious diet possible, so skipping these foods will likely leave your nutritional intake overly limited.
In exploring the integration of these moderately tolerated foods into your routine, you’ll want to be aware of portion size and frequency and how these affect your gut. For example, you might find that small servings of moderately tolerated foods every few days are just fine, but larger servings are not. Or you may find that you can eventually eat certain foods daily, but not multiple times per day, due to FODMAP stacking effects. Take your time and try not to rush, so you can more clearly see cause and effect while also continuing to add more delicious foods to your day.
Consider Your Approach to Poorly Tolerated Foods
You will likely not want to include large servings of poorly tolerated foods into your diet in order to avoid symptoms, however in some cases, there are times you may want or need to (such as when eating out, traveling, visiting friends and family, etc.). In these situations, it may be best to limit FODMAP intake over other parts of the day, to minimize stacking and reduce the risk of exceeding your threshold in a major way.
In some scenarios, you can also trial digestive enzymes for certain poorly tolerated foods to enable eating a bit of these while reducing symptoms. For example, taking lactase (lactose), alpha-galactosidase (GOS, fructans), xylose isomerase (fructose) or inulinase (oligo-saccharides) may aid in digestion for foods in these FODMAP categories. It’s important to note that the effect of digestive enzymes can be modest, so trialing these in a “safe environment” (at home or with small quantities of poorly tolerated foods) may be best to assess your specific outcomes.
Consider Using the Filtering Feature in the Monash Low FODMAP Diet (LFD) App
The Monash LFD app’s filtering capability offers an easy way to identify foods and portion sizes that fit your unique tolerances. Using the filtering feature, you simply identify your level of tolerance (green, which equal well-tolerated foods; yellow, which are moderately tolerated foods or red, which are poorly tolerated foods) for each FODMAP group, and the app will show you proper portion sizes, as well as foods to avoid. This can be very handy in the grocery store or when eating out, as well as during meal planning, to enable you to comfortably eat a wide variety of foods while keeping an eye on those that may be troublesome for your gut.
Eat Plenty of Low-to-No FODMAP Foods!
While you’re still testing the waters of your newfound low FODMAP freedom, you will also want to ensure you have plenty of nutritious and delicious options to choose from. Remember that there are lots of non-FODMAP-containing foods out there, as well as many with just a trace of FODMAPs, for you to choose from. In general, these foods do not need to be limited and can be combined freely in meals and snacks.
Some examples include:
- Fruits (yellow bananas, breadfruit, clementines, dragon fruit, durian melon, grapes, guava, navel oranges, papaya, plantain, prickly pear, rhubarb, starfruit, and strawberries).
- Grains (rice, quinoa)
- Nuts (Macadamia nuts, peanuts)
- Oils (ex. avocado, canola, coconut, olive, peanut, sesame, sunflower, vegetable oil, walnut oil, etc.).
- Other fats, such as butter, margarine, and duck fat.
- Protein foods (beef, egg whites, fish, lamb, poultry, shellfish).
- Vegetables (arugula, bamboo shoots, mung bean sprouts, pickled beetroot, carrot, choy sum, cucumber, endive, galangal, pickled jalapeno, Japanese pumpkin, kale, lettuce, pattypan squash, olives, parsnip, potatoes, red bell pepper, red radish, green scallion tops, Swiss chard, canned and drained tomatillos, and common beefsteak tomato.
Address Nutritional Gaps
You may have found that you poorly tolerate one or more major food groups during the Challenge Phase. For example, poor tolerance of lactose can dramatically reduce your dairy food options. Or perhaps you do not tolerate fructose very well, putting a large variety of fruits into your gut’s “no thanks” category.
This is where we want to take a close look at overall dietary variety and seek out low FODMAP swaps for higher FODMAP foods and/or assess how best we can meet our overall nutritional needs, while still maintaining good levels of symptom control.
Generally, this part of the Integration Phase may be best undertaken in consultation with a registered dietitian, to help identify nutrient-rich foods that won’t upset your gut and/or dietary supplements that can ensure you reach your daily requirements.
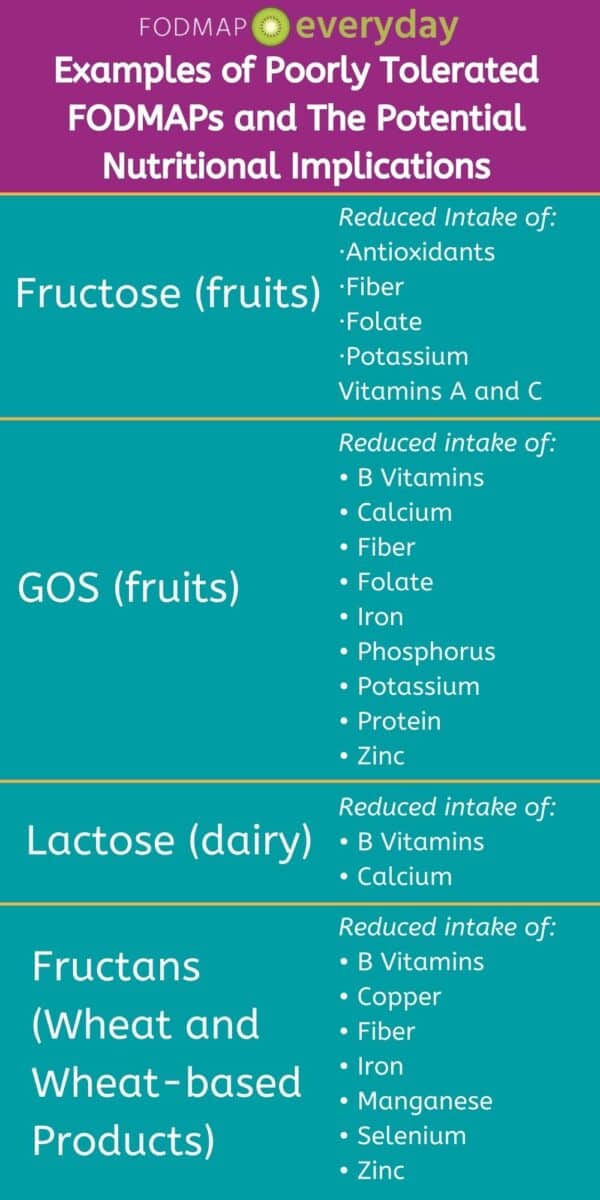
However, if you don’t have access to a dietitian, the table below outlines a few potential nutritional gaps that can arise from limited intake of certain FODMAP groups. (Note: This list is not all-inclusive. To read more about how to address some of these nutritional concerns, see my article “Nutritional Deficiencies and the Low FODMAP Diet”).
The Takeaway
With just a bit of patience and lots of continued curiosity, during the Integration Phase you’ll soon be able to expand your diet significantly and enjoy eating a wider variety of foods without fear of uncomfortable symptoms. However, it is important to remember that IBS responds not only to FODMAPs – you’ll still want to be aware of other potential triggers in your life, such as stress, hormonal changes, intense exercise, medications, spicy or fatty foods, alcohol, and even fluid intake.
It’s also important to note that tolerances can change over time, so while the Integration Phase essentially becomes your “new normal,” in terms of foods you can eat comfortably and regularly, you may want to go back and re-test moderately or poorly tolerated foods at some point in the future (we typically recommend this after about 6 months) to see if there are still more foods that you can integrate back into your eating routine.
Also, we know that occasionally you might have to pause your progression through the 3 phases of the diet. Please take a look at our article, Pausing The Low FODMAP Diet