Let’s Talk About the “D” in FODMAP
The “D” in FODMAP stands for disaccharide, and it specifically refers to one particular disaccharide, namely lactose.
The Monash University researchers who created the low FODMAP diet chose to use a “D” instead of an “L” in order to maintain consistency throughout the acronym by using the first letter of the carbohydrate group that each FODMAP belongs to.
The Chemistry of the “D” in FODMAP
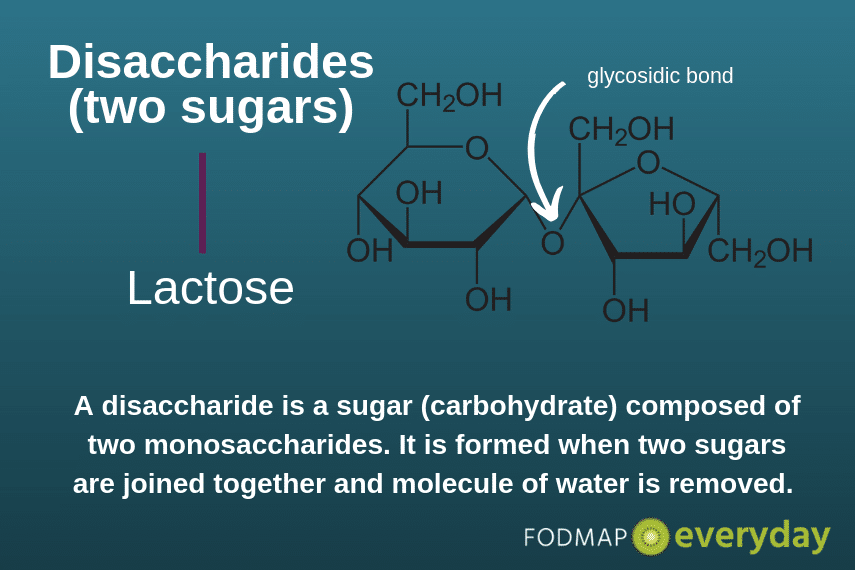
Disaccharides are small chain carbohydrates that consist of two monosaccharides (“simple” sugars”) joined by a glycosidic bond. The monosaccharides that make up lactose are galactose and glucose.
What Causes Lactose Malabsorption?
Lactose malabsorption is caused by the body’s inability to produce enough lactase, the enzyme needed to break the bond between the two sugar molecules that comprise lactose.
Instead, intact lactose travels through the small intestine attracting water via a process called osmosis and ultimately lands in the large intestine where it is fermented by gut bacteria.
Both the excess water and the gas produced by bacterial fermentation of undigested lactose push on the walls of the large intestine, causing symptoms in people who are lactose intolerant (this term refers to people who experience symptoms when they consume lactose, which is not the case for all those who malabsorb this sugar).
Some people actually have the ability to make sufficient lactase but are unable to do so because of an underlying condition that damages the small intestinal villi, which are the source of this enzyme.
The most common causes of this secondary lactose intolerance are untreated celiac disease and gastroenteritis. Secondary lactose intolerance is usually temporary, and will reverse over time once the underlying issue is addressed.
Symptoms of Lactose Intolerance
Lactose intolerance causes symptoms that are very similar to IBS, namely pain, bloating, gas, and diarrhea. Because of the overlap between these two conditions, you may want to try cutting out all lactose-containing foods for at least three days before embarking on the Elimination Phase of the low FODMAP diet.
If your symptoms resolve with just this intervention, you may not need to restrict the other FODMAPs!
Testing for Lactose Intolerance
The two most widely used diagnostic tests for lactose intolerance are the hydrogen breath test and a lactose restricted diet followed by a “test-to-tolerance” protocol (like the Challenge Phase of the low FODMAP diet).
The hydrogen breath test is quick and easy, but many gastroenterologists and dietitians prefer the dietary approach because they believe it provides more reliable results.
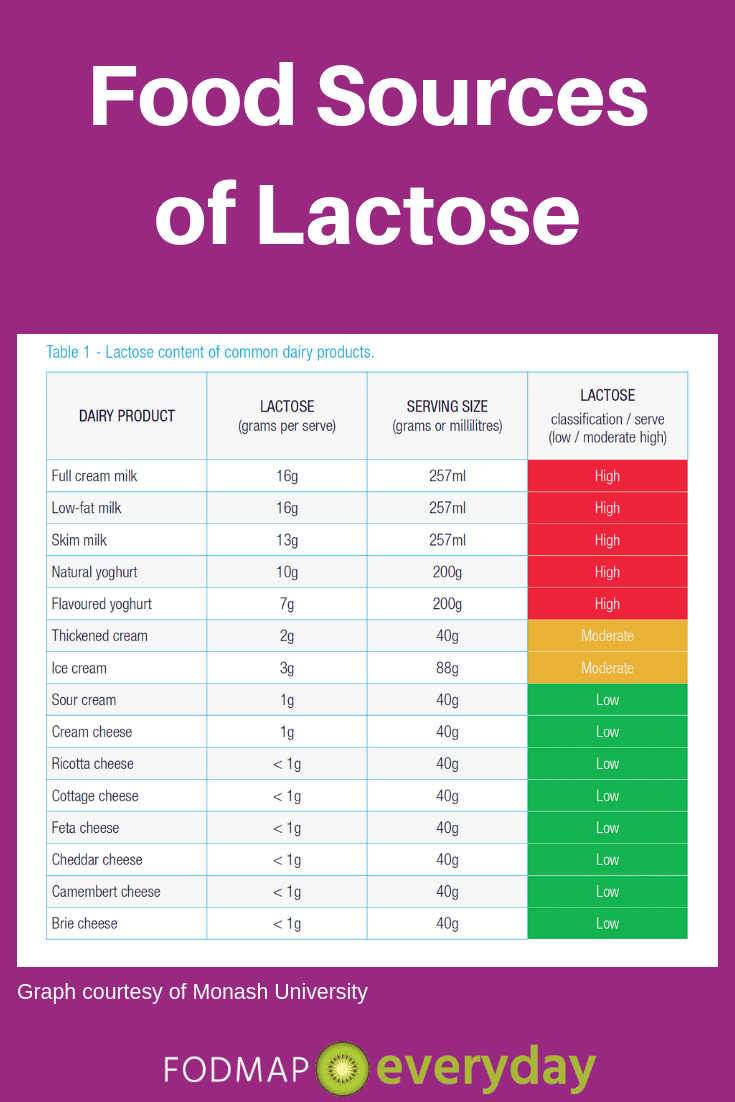
Food Sources of Lactose
Lactose is often referred to as “milk sugar” because it is found in milk and milk products, such as yogurt, ice cream, and certain cheeses. Milk from cows, goats, and sheep all contain significant amounts of lactose unless it’s formulated with lactase enzyme, such as lactose-free milk.
Fermented dairy foods, such as yogurt and kefir, are lower in lactose than regular milk, and aged cheese is virtually lactose-free. That’s because bacteria added to milk during the processing of these foods has a similar action as lactase – it breaks down the lactose molecule into easily absorbed simple sugars.
Health Benefits of Lactose
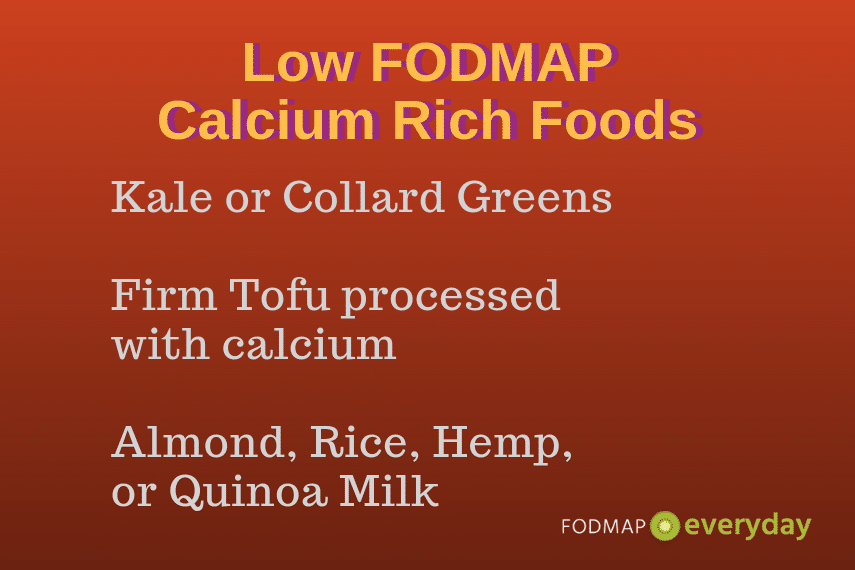
The primary health benefit of lactose lies in the food in which it is contained. Milk and milk products are an excellent source of bioavailable calcium and high-quality protein. If you are avoiding dairy due to lactose intolerance, it is imperative that you get your calcium from other dietary sources (see graphic below) or supplements.
Or, check out our article on DIY Lactose-Free Dairy to learn how to make your own lactose-free milk, cream, half and half and more. Likewise, if dairy foods were a significant source of protein for you, please include other protein-rich items to make up for the shortfall.
Bottom Line
Lactose intolerance exists on a spectrum. Many people do just fine with aged cheeses and other fermented dairy foods, and research suggests that most people with lactose intolerance can tolerate 12 to 15g of lactose per day, which is approximately the amount in 1 cup (240 ml) of milk. Hint: if you spread your consumption throughout the day, you might be able to tolerate more!
If you discover that you are extremely sensitive to lactose, there are plenty of lactose-free milk products on the market these days, such as milk, half-and-half, cream cheese, sour cream and more,
Alternately, you can opt for calcium-rich vegetables like kale or collard greens, firm tofu processed with calcium, or almond, hemp, quinoa or rice milk (all of which are low FODMAP in appropriate serving sizes).
You can also try taking a low FODMAP formulation of a lactase enzyme supplement immediately prior to consuming dairy foods.
For more on lactose and the Low FODMAP diet, check out this article by Success Team member Rachelle LaCroix Mallik.
Be sure to read all of the other articles in this series!






Why would I only be able to tolerate a low (25gm) serve of lactose free plain yoghurt per day? Prior to a bowel resection 4 years ago I tolerated lactose well, and I can tolerate other lactose free products in reasonable serves. Is there a way to build up tolerance for yoghurt?
Do you have a detailed, with photos, post on collard greens? It isn’t a familiar thing in Australia – maybe it comes under another term? Anything you can tell me is welcome!
Thanks, Jo
Hi Jo, apparently Collards are called Borekale in Australia. I learned something new – thank you:) As far as building up tolerance, certainly ask a dietitian but also take a look at this article by a MD who discusses how we can “train” our gut in some instances. It is fascinating.