Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects millions of people worldwide. However, its symptoms can be similar to those of several potentially life-threatening conditions. Too many people think they have a “tummy ache” or that their “stomach hurts” and thinking along these lines will lead them down the wrong diagnostic path. The similarity of numerous very serious medical conditions with IBS underscores the critical importance of seeking professional medical advice rather than attempting self-diagnosis.
What Are The Most Common Conditions That Mimic IBS?

The most common conditions that mimic IBS include: inflammatory bowel disease (IBD), celiac disease, colon cancer, diverticulitis, intestinal ischemia, lactose intolerance, small intestinal bacterial overgrowth (SIBO), and endometriosis.
A Closer Look At Diseases That Look Like IBS

There are several medical conditions. Let’s take a look:
Inflammatory Bowel Disease (IBD)

IBD, which includes Crohn’s disease and ulcerative colitis, is a group of chronic inflammatory conditionsaffecting the gastrointestinal tract. While IBS and IBD share some symptoms, IBD is characterized by inflammation and can lead to severe complications.
Symptoms:
- Abdominal pain
- Diarrhea
- Constipation
- Rectal bleeding
- Weight loss
- Fever
Key Characteristics:
IBD is characterized by chronic inflammation of the gastrointestinal tract and includes conditions like Crohn’s disease and ulcerative colitis. Symptoms typically include abdominal pain, diarrhea, rectal bleeding, and weight loss. The disease often presents with periods of active symptoms alternating with remission. IBD can be associated with extra-intestinal manifestations affecting joints, skin, and eyes. Diagnosis usually involves a combination of clinical evaluation, imaging studies, and endoscopy.
Potential Consequences:
IBD can cause permanent damage to the intestines and increase the risk of colon cancer1. It may also lead to complications such as bowel obstruction, malnutrition, and in severe cases, life-threatening sepsis.
Colon Cancer
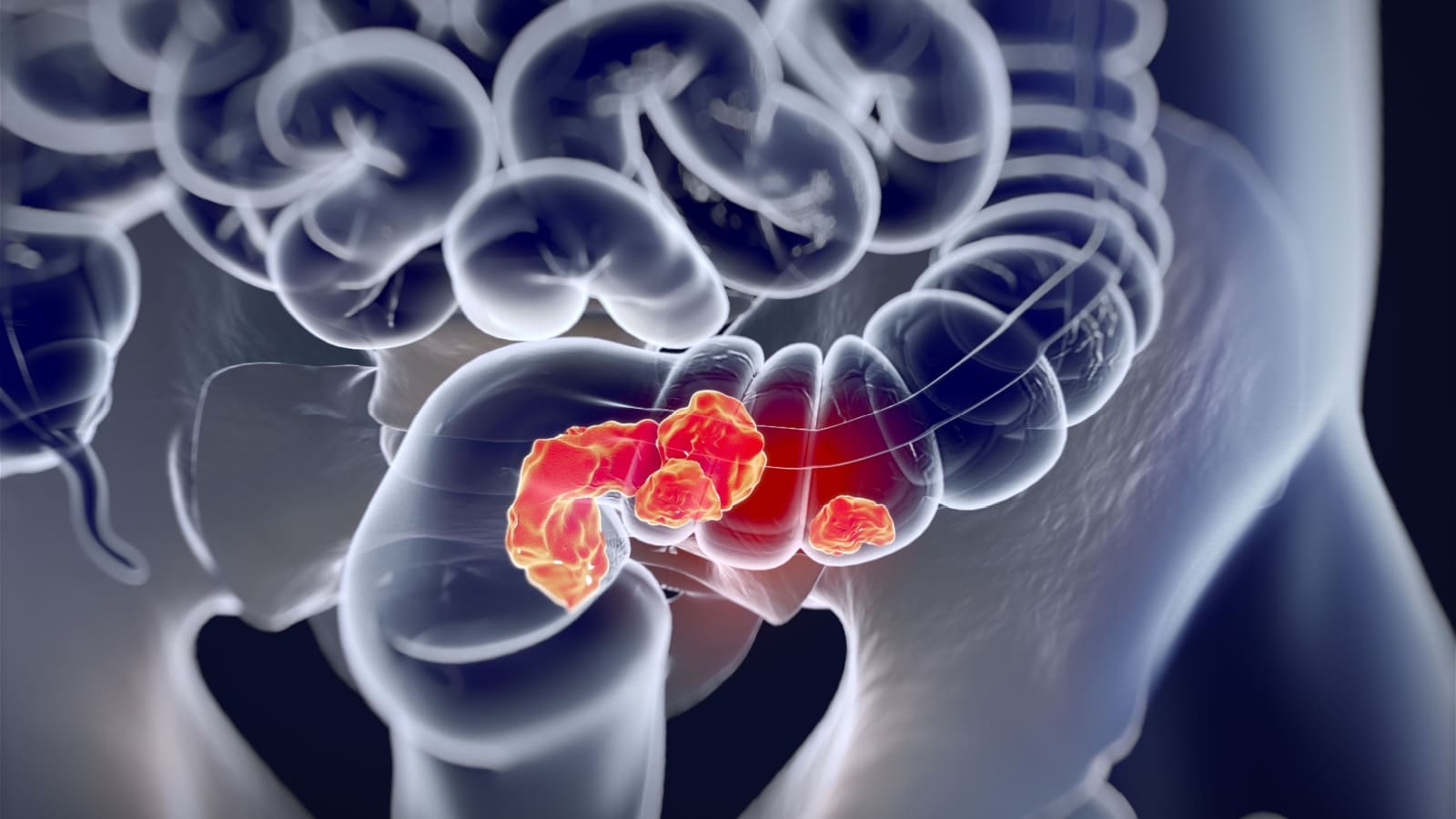
Colon cancer is a serious condition that can initially present with symptoms similar to IBS.
Symptoms:
- Changes in bowel habits
- Abdominal pain
- Rectal bleeding
- Unexplained weight loss
Key Characteristics:
Colon cancer often develops slowly over several years and may present with changes in bowel habits, rectal bleeding, and abdominal discomfort. It can cause unexplained weight loss and fatigue. The risk of colon cancer increases with age, especially after 50. Importantly, it may be asymptomatic in early stages, which emphasizes the importance of regular screenings. Diagnosis is confirmed through colonoscopy and biopsy. Early detection significantly improves prognosis and treatment outcomes, making timely medical evaluation crucial for any persistent changes in bowel habits or unexplained gastrointestinal symptoms.
Potential Consequences:
If left undiagnosed and untreated, colon cancer can spread to other parts of the body, significantly reducing survival rates. Early detection is crucial for successful treatment.
Celiac Disease

Celiac disease is an autoimmune disorder triggered by gluten consumption.
Symptoms:
- Abdominal pain
- Diarrhea
- Bloating
- Fatigue
- Joint pain
- Skin rashes
Key Characteristics:
Celiac disease is triggered by gluten consumption in genetically predisposed individuals. It presents with a wide range of symptoms, including abdominal pain, diarrhea, and bloating. Notably, it’s often associated with non-gastrointestinal symptoms like fatigue and joint pain. If left untreated, celiac disease can lead to malabsorption and nutritional deficiencies. Diagnosis is typically made through blood tests and intestinal biopsy. Management involves strict adherence to a gluten-free diet, which can dramatically improve symptoms and prevent complications.
Potential Consequences:
Untreated celiac disease can lead to malnutrition, osteoporosis, infertility, and an increased risk of certain cancers.
Diverticulitis

Diverticulitis occurs when small pouches in the colon become infected or inflamed.
Symptoms:
- Abdominal pain (usually in the lower left side)
- Fever
- Nausea
- Vomiting
- Changes in bowel habits
Key Characteristics:
Diverticulitis is marked by an acute onset of abdominal pain, usually localized in the lower left quadrant. It’s often accompanied by fever, nausea, and changes in bowel habits. Patients may experience tenderness in the affected area. This condition is more common in older adults and those with low-fiber diets. In severe cases, diverticulitis can lead to complications such as abscesses or bowel perforation, requiring immediate medical attention.
Potential Consequences:
Severe cases of diverticulitis can lead to bowel perforation, abscess formation, or peritonitis, all of which are life-threatening conditions requiring immediate medical intervention.
Intestinal Ischemia

Also referred to as mesenteric ischemia, his condition results from reduced blood flow to the intestines.
Symptoms:
- Sudden, severe abdominal pain
- Bloody diarrhea
- Nausea
- Vomiting
Key Characteristics:
Intestinal ischemia is characterized by a sudden onset of severe abdominal pain, often disproportionate to physical exam findings. In chronic cases, pain typically worsens after eating. The condition can occur acutely or develop gradually over time, and may present with nausea, vomiting, and bloody stools. It often affects older adults, especially those with cardiovascular risk factors. If left untreated, intestinal ischemia can lead to serious complications like bowel necrosis and peritonitis.
Potential Consequences:
Intestinal ischemia can quickly lead to tissue death (necrosis) in the affected area. Without prompt treatment, it can cause bowel perforation, sepsis, and death.
Lactose Intolerance

Lactose intolerance is a common digestive disorder that can present symptoms similar to IBS.
Symptoms:
- Bloating
- Abdominal pain
- Diarrhea
- Gas
Key Characteristics:
Lactose intolerance occurs when the body cannot properly digest lactose, a sugar found in milk and dairy products. One in three people with IBS don’t feel good after they eat dairy products, indicating a potential overlap between these conditions.
Potential Consequences:
While not life-threatening, lactose intolerance can significantly impact quality of life and lead to nutritional deficiencies if dairy products are completely eliminated without proper substitution.
Small Intestinal Bacterial Overgrowth (SIBO)

SIBO is a condition characterized by an abnormal increase in the bacterial population in the small intestine.
Symptoms:
- Abdominal pain
- Bloating
- Diarrhea
- Malabsorption
- Unintentional weight loss
Key Characteristics:
SIBO occurs when bacteria that normally reside in the large intestine overgrow in the small intestine3. It can be caused by complications of abdominal surgery, structural problems in the small intestine, or certain medical conditions that slow intestinal motility.
Potential Consequences:
If left untreated, SIBO can lead to malnutrition, weight loss, and osteoporosis5. It can also cause inflammation in the intestinal mucosa, exacerbating symptoms.
Endometriosis

Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus.
Symptoms:
- Pelvic pain
- Painful periods
- Pain during intercourse
- Gastrointestinal symptoms (similar to IBS)
Key Characteristics:
Endometriosis can cause gastrointestinal symptoms that mimic IBS. Interestingly, there’s a significant connection between endometriosis and SIBO. Studies have shown that 100% of endometriosis patients had small intestinal motility issues, which predispose to SIBO development.
Potential Consequences:
Endometriosis can lead to chronic pain, fertility issues, and a decreased quality of life. The connection with SIBO can exacerbate digestive symptoms.
The Interconnection

It’s important to note that these conditions can coexist and even influence each other. For instance:
- People with endometriosis are more likely to develop SIBO.
- Both SIBO and endometriosis can cause symptoms similar to IBS, leading to potential misdiagnosis.
- Lactose intolerance can exacerbate symptoms in people with IBS or SIBO.
Given these complex interactions, it’s crucial to seek professional medical advice for accurate diagnosis and appropriate treatment. Self-diagnosis or misdiagnosis can lead to inadequate treatment and prolonged suffering.
The Dangers of Self-Diagnosis

Given the overlap in symptoms between IBS and these potentially deadly conditions, self-diagnosis can be extremely dangerous. Here’s why:
- Missed Diagnoses: Self-diagnosing as IBS might lead to overlooking more serious conditions. For instance, dismissing bloody stools as a symptom of IBS could delay the diagnosis of colon cancer or IBD.
- Delayed Treatment: Many of the conditions that mimic IBS require prompt medical intervention. Delaying treatment due to misdiagnosis can lead to disease progression and more severe outcomes.
- Inappropriate Self-Treatment: Attempting to treat self-diagnosed IBS with over-the-counter medications or dietary changes may be ineffective or even harmful if the underlying condition is something more serious.
- Psychological Impact: Living with undiagnosed symptoms can cause significant anxiety and stress, which may exacerbate existing health issues.
- Misinterpretation of Symptoms: Many symptoms can be subtle or easily misinterpreted. For example, the abdominal pain of intestinal ischemia might be mistaken for IBS-related discomfort.
The Importance of Professional Medical Diagnosis

Consulting with healthcare professionals is crucial for several reasons:
- Expertise and Experience: Doctors have the training and experience to differentiate between IBS and more serious conditions. They can recognize subtle signs and symptoms that a layperson might miss.
- Access to Diagnostic Tools: Healthcare providers can order and interpret necessary tests, such as blood work, stool samples, imaging studies, and endoscopies, to accurately diagnose the underlying condition.
- Comprehensive Health Assessment: Doctors consider your entire health history, family history, and lifestyle factors when making a diagnosis. This holistic approach is crucial for accurate diagnosis and effective treatment.
- Appropriate Treatment Plans: Once a correct diagnosis is made, healthcare providers can recommend appropriate treatment strategies, whether it’s medication, dietary changes, or more intensive interventions.
- Monitoring and Follow-up: Regular check-ups allow doctors to monitor your condition, adjust treatments as necessary, and catch any changes or complications early.
- Psychological Support: Dealing with chronic gastrointestinal issues can be emotionally taxing. Healthcare providers can offer support or refer you to mental health professionals if needed.
Do NOT Self-Diagnose

While IBS is a common and generally non-life-threatening condition, its symptoms can mimic those of several potentially deadly diseases. Conditions such as inflammatory bowel disease (IBD), colon cancer, celiac disease, diverticulitis, and intestinal ischemia all share symptoms with IBS but can have severe, even life-threatening consequences if left undiagnosed and untreated.
The dangers of self-diagnosis cannot be overstated. Misinterpreting symptoms or dismissing them as “just IBS” can lead to delayed treatment, disease progression, and poorer outcomes.
Who Should Do The Diagnosing?

Several types of medical professionals are particularly skilled at diagnosing conditions that mimic Irritable Bowel Syndrome (IBS) and IBS itself. The most prominent among these are:
Gastroenterologists

Gastroenterologists are specialists in digestive diseases and are often the most qualified to diagnose IBS and related conditions. They have extensive training in recognizing the nuances of gastrointestinal disorders and can perform specialized tests such as endoscopies and colonoscopies.
Gastroenterologists are adept at:
- Interpreting complex symptom patterns
- Ordering and analyzing appropriate diagnostic tests
- Distinguishing IBS from more serious conditions like inflammatory bowel disease (IBD) or colon cancer
Primary Care Physicians

Primary care physicians often serve as the first point of contact for patients experiencing IBS-like symptoms. They can:
- Conduct initial evaluations and physical examinations
- Order preliminary blood tests and stool samples
- Refer patients to specialists when necessary
Internists

Internists, who specialize in adult medicine, can also play a crucial role in diagnosing IBS and related conditions. They are trained to:
- Evaluate a wide range of symptoms
- Consider the patient’s overall health and medical history
- Coordinate care with specialists if needed
Colorectal Surgeons

While not typically the first line for IBS diagnosis, colorectal surgeons may become involved if there are concerns about more serious conditions like colon cancer, especially in patients over 50 or those with a family history of colorectal cancer.
Endocrinologists

For conditions that may mimic IBS but have hormonal components, such as thyroid disorders, an endocrinologist might be consulted to provide specialized insight and testing.
A Collaborative Approach Is Best

It’s important to note that the diagnosis of IBS often involves a collaborative approach. While gastroenterologists are generally considered the most specialized in diagnosing IBS, the initial suspicion may come from a primary care physician or internist. These doctors work together, often starting with less invasive tests and progressing to more specialized examinations as needed.
Regardless of the specific type of doctor, the key to accurate diagnosis lies in their ability to recognize patterns of symptoms, conduct appropriate tests, and rule out more serious conditions. Patients over 50 or those with red flag symptoms such as unexplained weight loss, anemia, or blood in the stool should be particularly thorough in their medical evaluations.
Now What? Get A Registered Dietitian!

Registered Dietitians (RDs) play a crucial role in managing various gastrointestinal conditions that mimic IBS. Their specialized expertise allows them to create personalized nutrition plans tailored to specific digestive disorders. Please note that the term “nutritionist” is unregulated in the U.S. You want a “Registered Dietitian”.
RDs work closely with gastroenterologists to provide comprehensive care. They conduct thorough assessments, including food diaries and symptom tracking, to identify trigger foods and create individualized plans. Their approach often involves a combination of elimination diets, such as the low FODMAP diet, specialized nutrition protocols, and lifestyle modifications to manage symptoms effectively.
Dietitians Provide Ongoing Support That Doctors Do Not

By providing ongoing support and education, RDs empower patients to make informed decisions about their diet and lifestyle, leading to improved symptom management and overall quality of life. Their expertise in navigating complex dietary restrictions while maintaining nutritional balance is invaluable in the long-term management of these gastrointestinal conditions.
Conclusion

Only healthcare professionals have the knowledge, tools, and experience to accurately differentiate between IBS and more serious conditions.
Therefore, if you’re experiencing persistent gastrointestinal symptoms, it’s crucial to seek medical attention.
A doctor can perform the necessary examinations and tests to determine the true cause of your symptoms and recommend appropriate treatment. A Registered Dietitian will help with the necessary dietary and lifestyle changes. Remember, when it comes to your health, it’s always better to err on the side of caution and seek professional medical advice. Your life may depend on it.





