Not the sexiest of topics, but diarrhea is a life-altering problem for many individuals, including those with IBS-D (diarrhea-predominant IBS). A lot of my patients are afraid to leave their homes for fear of being away from a bathroom.
Hoping to manage diarrhea, many people with IBS-D put themselves on overly restrictive, nutrient deficient, unsustainable diets. Part of my job as a GI dietitian is to help patients normalize their bowels with as few dietary restrictions as possible, if at all.
To treat diarrhea, we have to know what’s causing it. Without that, it’s impossible to fix. The low FODMAP diet is one way to treat symptoms of IBS-D, but sometimes there are more suitable strategies. This article will explore potential causes of IBS-related diarrhea, discuss everyday triggers, and offer actionable solutions.
What is Diarrhea?
OK, this might seem like a simple question with an obvious answer. However, a patient’s notion of diarrhea might differ from the medical definition.
In the clinical setting, diarrhea means loose watery stools three or more times per day. Stool consistency is between types 5 and 7 on the Bristol stool chart. Passing frequent hard stool or pellet-like stool is not diarrhea, although patients often report it so because they spend much of their life in the bathroom.
Diarrhea lasting more than four weeks is chronic, whereas diarrhea persisting less than 2 weeks is acute. IBS-D is a top cause of chronic diarrhea and the focus of this article. However, chronic diarrhea can stem from other conditions, so it’s important to see a doctor and not self-diagnose.
Here’s a partial list of health conditions associated with chronic diarrhea:
- Bile acid diarrhea (discussed below)
- Celiac disease
- Crohn’s diseases
- Dumping syndrome
- Hyperthyroidism
- Microscopic colitis
- Pancreatic disease
- Ulcerative colitis
- Previous abdominal surgery
- Small intestinal bacterial overgrowth (discussed below)
Diarrhea and IBS
Irritable bowel syndrome (IBS) is a disorder of the brain-gut interaction that affects about 10-15% of the world’s population. In IBS, the bowel is exactly as it sounds… irritable.
You may want to read: What is IBS?
We have much to learn about IBS-D, but here are some major reasons someone with IBS might suffer from diarrhea:
Rapid Intestinal Transit
Stool is normally liquid when it arrives in the colon, its last stop before it plunges to its final destination. In healthy individuals, the stool solidifies as it travels throughout the colon. That’s because your colon dehydrates the stool by reabsorbing fluid. However, in people with IBS-D, rapid intestinal transit doesn’t allow the colon enough time to reabsorb the water. Hence, the resulting watery stool or diarrhea.
People with IBS-D often report frequent loose stools in the morning shortly after waking and/or after eating. It’s not uncommon for people with IBS-D to report the feelings of food “running right through” them. Sometimes they have to run to the bathroom mid-meal. If this happens to you, you can probably thank your gastrocolic reflex.
Gastrocolic Reflex
The gastrocolic reflex is a normal physiological response to food. When food enters the stomach, the stomach sends a message to the colon to make room because there’s more food coming. The colon responds by speeding up motility to clear space for the incoming load. Some people with IBS have an exaggerated gastrocolic reflex, which can lead to urgent loose bowel movements after eating.
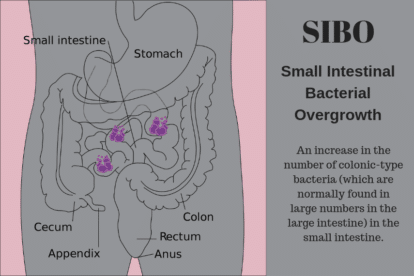
SIBO: Small Intestinal Bacterial Overgrowth
Researchers suspect an altered gut microbiome (dysbiosis) plays a role in IBS. One type of dysbiosis that can worsen diarrhea is small intestinal bacterial overgrowth (SIBO).
SIBO is exactly what it sounds like — excessive amounts of bacteria in the small bowel. Typically, these are colonic microbes that wander from the large to the small intestine in search of food. SIBO is highly prevalent in IBS and may be responsible for IBS-D in some individuals.
You May Want To Read: SIBO – Get the Facts
Risk factors for SIBO in patients with IBS-D include excess antibiotics, diverticulosis, long-term use of proton pump inhibitors (PPIs) and gastroenteritis.
If you have diarrhea and bloating soon after eating high-fat or high FODMAP foods, ask your health care provider about SIBO breath testing.
Bile Acid Diarrhea
Roughly one-third of people with IBS-D suffer from bile acid diarrhea. Bile acids help us digest and absorb dietary fats. Afterwards they’re recycled in the small intestine. However, some conditions inhibit bile acid reabsorption so they pass on to the colon where they speed up colonic transit and promote water and electrolyte secretion, resulting in diarrhea.
Bile acid diarrhea can occur for reasons other than IBS (e.g. gallbladder removal, Crohn’s ileitis), but put it on your radar, especially if you don’t respond to standard IBS therapy.
Carbohydrate Intolerance
Maldigestion or malabsorption of polyols, lactose, fructose and/or sucrose can cause diarrhea. Unabsorbed sugars draw water into the bowel leading to osmotic diarrhea. This can occur because of an enzyme deficiency and/or a lack of transporters to escort the sugars into the body. Gas and/or bloating usually accompany diarrhea. See “the section on dietary triggers, below.
IBS-D Triggers & Management
Diet
Often, patients with IBS-D blame their diarrhea on something they ate and turn towards dietary changes to control their symptoms. Without a doubt, food can worsen IBS symptoms, but food does not cause IBS.
While dietary triggers vary from person to person, these are some of the worst offenders for IBS-D:
Fatty Foods:
Fat triggers the gastrocolic reflex and bile acid secretion, so it can worsen diarrhea in people with an exaggerated gastrocolic reflex and/or bile acid diarrhea. My patients tolerate plant fat (e.g. avocado, nut butters) better than animal fat.
- Examples: Fried foods, animal fat (e.g. burgers), high-fat dairy (e.g. cream-based soups, milkshakes), greasy/oily foods
- What to choose instead: Baked foods, lean meats, low-fat dairy, vegetables, fruits
Coffee:
Coffee contains cholinergic acid, which stimulates colonic activity.
- Examples: Coffee, both decaf and caffeinated
- What to choose instead: Tea, herbal tea, hot water with lemon.
You May Want To Read: Tea & FODMAPs and IBS, The Low FODMAP Diet, Coffee & Coffee Drinks
Insoluble fiber:
Also called roughage because of its coarse nature, foods with insoluble fiber generate water and mucus secretion in the colon.
- Examples: Popcorn, raw vegetables, whole nuts and seeds, vegetable skins and stalks, fruit skins and seeds
- What to choose instead: Peeled fruits and vegetables, cooked vegetables, nut and seed butters, corn chips
You May Want To Read: Fiber and IBS: What You Need To Know
Alcoholic beverages:
Alcohol inhibits colonic absorption of water and can lead to fat malabsorption. My patients rank beer as the worst culprit in this category. Beer sends more unabsorbed carbohydrates to the colon, where they act as a laxative.
- Examples: Wine, beer, liquor.
- What to choose instead: A low-sugar mocktail, like this Cucumber Mint Lime Agua Fresca
You May Want To Read: Drinking Alcohol On The Low FODMAP Diet
Sugary drinks:
Everyone has a limit for how much sugar they can digest and absorb. People with IBS-D are more vulnerable to excess sugar. Sugary drinks are astonishingly high in sugar.
- Examples: Soda, sweetened iced tea, lemonade, nutritional shakes, sports drinks, juice
- What to choose instead: Watered down juice, water with lemon, unsweetened iced tea, flavored water, homemade oral rehydration solutions, homemade low-sugar smoothies
I don’t recommend anyone replace sugary drinks with artificially sweetened beverages, such as diet soda. Not only can artificial sweeteners worsen IBS symptoms, but research shows they might negatively affect the gut microbiota.
Those at risk for severe dehydration might require an oral rehydration drink with a combination of sugar and salt, but you’ll need much less sugar than most sugar-sweetened beverages, like sports drinks, provide. Try making your own oral rehydration solution from household staples, or test out a rehydration powder, like Ceralyte.
Spicy foods:
Capsaicin, an active ingredient in hot spices and peppers, can irritate the GI tract.
- Examples: chili peppers, cayenne, hot sauce
- What to choose instead: fresh herbs, smoked paprika, garlic-infused oil
You May want To Read: All About Chile, Chili & Chilli & The Low FODMAP Diet
FODMAPs:
Not everyone with IBS-D needs to be on a low FODMAP diet, but it can help. Beware of osmotically active FODMAPs, including polyols (sorbitol, mannitol), fructose and lactose.
- Examples of foods with added polyols: “sugar-free” gum, “sugar-free” gummy bears, “sugar-free” cookies, meal replacements
- Example of foods with naturally occurring polyols: Prunes, watermelon
- Examples of foods with lactose: milk, ice cream, frozen yogurt, soft cheeses (e.g. ricotta)
You may want to read: What are FODMAPs?
Dietary management for chronic diarrhea isn’t just about what you eat, it’s about how you eat and how much you eat. Large meals stimulate the gastrocolic reflex more than small meals, so small, frequent meals might be the way to go. Chewing and eating slowly is important for digestion. I can’t count the number of times a patient has told me that the best thing they did to manage their diarrhea was to eat slowly and mindfully. Small changes lead to big results.
Medications & Supplements
Beware that some medications can worsen diarrhea, whereas others can help.
Doctors prescribe these medications to help IBS-D:
- Xifaxan (rifaximin) — commonly used to treat SIBO
- Antispasmodics and anticholinergics
- Tricyclic antidepressants (TCAs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Viberzi (eluxadoline)
- Bile acid binders — used to treat bile acid diarrhea
You can work with your doctor to determine if any of these are appropriate for you.
These medications might worsen diarrhea:
- Antibiotics
- Antidepressants
- Blood pressure medications (e.g. ACE inhibitors)
- Metformin
- Proton Pump Inhibitors (e.g. Nexium, Prevacid)
- Magnesium containing products
Do not discontinue medications without speaking with your doctor.
Like medications, supplements can help or hinder IBS-D. Watch out for high dose vitamin C, high dose magnesium and insoluble fiber supplements as these can worsen diarrhea. Some soluble fiber supplements, such as psyllium seed husk, can help form stool and reduce symptoms of IBS-D.
As for probiotics… they might help, but it’s trial and error. The US Probiotic Guide offers a list of probiotics for IBS, but not IBS-D, specifically. If you are in the Elimination or Challenge Phase of the low FODMAP diet, please do not add probiotics to your diet without consulting with your dietitian; they can make it difficult to assess FODMAP triggers, which is what these early phases are all about.
Note! Not only can active ingredients in drugs and supplements worsen diarrhea, but so can their inactive “filler” ingredients. Many of these fillers are FODMAPs, including lactose, sorbitol, mannitol and polydextrose.
What Else?
A note on stress… Stress doesn’t cause IBS but it can worsen symptoms, including diarrhea. I tell all my patients that even if we could identify their perfect diet, it would only take them so far. Stress management is an important part of IBS treatment. Not sure where to start? How about gut-directed hypnotherapy, yoga, and/or meditation?
IBS & Yoga Series: Activating and Applying Your Self Knowledge
IBS & Yoga Series: Identifying Habits
IBS & Yoga Series: Kitchen Yoga
IBS and Yoga Series: Developing A Practice
IBS & Yoga Series Intro: It’s Your Body
IBS and Yoga Series: It’s Your Body — Where to Begin?
A note on Histamine…
Histamine is a natural component of some foods and found in human cells throughout the body. It’s an important part of the immune system and plays a role in many GI processes, including digestion. However, a histamine overload can trigger a variety of symptoms in certain individuals, including some people with IBS.
When someone with a histamine intolerance eats a high-histamine food or foods, they feel sick. High histamine foods span all the food groups, but common culprits include wine, cured meats, aged cheese and other fermented foods.
I’d be remiss not to mention histamine intolerance because I’ve worked with countless patients who searched high and low for a treatment for their diarrhea before they discovered a low histamine diet. NOTE: Please do not attempt a low histamine diet without guidance from a knowledgeable dietitian.
When To See A Doctor
If you have IBS-D, then you’ve likely come to expect diarrhea as part of your condition. And, while it can dramatically impair your quality of life, it’s not life-threatening. However, chronic diarrhea can stem from a more serious cause. Be sure to speak with your doctor if you experience any of the following:
- Significant unintentional weight loss
- Bloody, black or tarry stool
- Fecal incontinence
- Nocturnal diarrhea
- Fever
Key Takeaways
Living with diarrhea is not the answer to IBS-D. There are solutions, but first you and your healthcare team must identify why you’re having diarrhea. From there, you’ll be able to take small and deliberate steps towards feeling better — dietary or otherwise. In doing so, keep the following points in mind:
- There is no one “IBS diet.” The best approaches are personalized to your needs.
- Aim for the fewest dietary restrictions possible. A pleasurable, healthy and healing diet is full of variety.
- Do not put yourself on a gluten-free diet without ruling out celiac disease.
- Do yourself a big favor by working with a knowledgeable GI dietitian. Studies show that dietary interventions work best when they involve a RD.
- Scan your medicine cabinet for IBS triggers.
- Find a stress management technique that works for you. Dietary changes will only take you so far.
References
Andrews CN, Bradette M. Diarrhea-Predominant Irritable Bowel Syndrome: Medical Management Update. J Can Assoc Gastroenterol. 2019;3(6):e37-e48. Published 2019 Dec 3. doi:10.1093/jcag/gwz034
Camilleri M. Advances in understanding of bile acid diarrhea. Expert Rev Gastroenterol Hepatol. 2014;8(1):49-61. doi:10.1586/17474124.2014.851599
Camilleri M. Intestinal secretory mechanisms in irritable bowel syndrome-diarrhea. Clin Gastroenterol Hepatol. 2015;13(6):1051-e62. doi:10.1016/j.cgh.2014.07.020
Cangemi DJ, Lacy BE. Management of irritable bowel syndrome with diarrhea: a review of nonpharmacological and pharmacological interventions. Therap Adv Gastroenterol. 2019;12:1756284819878950. Published 2019 Oct 4. doi:10.1177/1756284819878950
Comas-Basté O, Sánchez-Pérez S, Veciana-Nogués MT, Latorre-Moratalla M, Vidal-Carou MDC. Histamine Intolerance: The Current State of the Art. Biomolecules. 2020;10(8):1181. Published 2020 Aug 14. doi:10.3390/biom10081181
Ochoa B, et al. Diarrheal Diseases – Acute and Chronic. American College of Gastroenterology. December 2012. Accessed December 2020. https://gi.org/topics/diarrhea-acute-and-chronic/#tabs2
Schiller LR. Nutrition management of chronic diarrhea and malabsorption. Nutr Clin Pract. 2006;21(1):34-39. doi:10.1177/011542650602100134
Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020;11:664. Published 2020 Jul 10. doi:10.3389/fpsyt.2020.00664