Are you an athlete with irritable bowel syndrome (IBS) and/or following a low FODMAP diet? Looking to improve recovery and get more out of your training while supporting your digestive health? Then this article is for you!
You know the feeling when you’ve had a hard or intense training session… You feel invigorated, but also know your body is going to hurt in different ways tomorrow and maybe for a few days after. What you do or do not eat can affect this recovery period – for better or worse.
Nutrition & Exercise

While you should be spacing out your intense workout days with active recovery and easier training days (please speak to a personal trainer and/or work with a specialized coach if you’re not sure how to balance this), your daily nutrition is of the utmost importance!
Proper nutrition can help you to recover from those workouts faster and have you feeling fresh for your next training session. Not to mention, recovery is essential to prevent injury, reduce risk of digestive flare-ups, as well as keep you motivated in the training process.
We did a deep dive on pre workout and post workout nutrition for active individuals with IBS in another article. You may want to read: Pre-Workout Nutrition and the Low FODMAP Diet and Post-Workout Nutrition and the Low FODMAP Diet.
This article provides a summary of what factors to consider on a daily basis to help support your performance and recovery while also managing your IBS and digestive health.
What Happens When We Exercise?
Exercise is defined as “a subset of physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness.” (1)
When we exercise, we put our body under stress – our central nervous system, cardiovascular system, muscles, etc. all work hard under the pressure and this leads to some natural damage to our muscle fibers as well as changes in heart rate, breathing and more. Our physiological systems change and adapt to the stress, and some of these changes lead to adaptation to exercise training over time. Essentially, when recovery conditions are optimal, the damaged muscle fibers repair and build up stronger!
The good news is that we can get a leg up on that adaptation with the RIGHT nutrition, as well as lifestyle habits. By doing what we can to maximize the recovery process, we can help our body to continue to recover from the stress we put it under with training demands, so that over time we will reap the results of our training.
Training vs. Working Out
You may exercise for general health reasons (mood, energy, sleep, digestion) and that is great. However, some people may use exercise to work towards a specific performance goal and therefore may be more inclined to maximize their recovery. They would take part in ‘training’ rather than working out or exercising. No matter which camp you’re in, if you’re looking to maximize your workouts to get stronger, recover better, and reduce risk of injury, then read on.
What is Exercise Recovery and Why Is It Important?

Put simply, recovery should allow you to enter your next training session as fit, if not more fit as you entered the previous one. Recovery is a process that involves reduction of inflammation and restoration that ultimately returns the body to homeostasis (aka a normal physiological state) after intense exercise and increased training loads (2).
Recovering poorly increases risk for illness and injury, as well as impacts gastrointestinal function. It can also impact your motivation and enjoyment of training and exercise. As the most extreme example, inadequate recovery on a regular basis can lead to overtraining syndrome.
Overtraining
Have you heard of overtraining syndrome? Put simply, overtraining can occur when increased training loads are not accompanied by adequate periods of rest and recovery. We need increased training loads to see improvements in performance (if you continue to train the same volume and intensity, then you won’t see much improvement), but adequate time and resources for adaptation between sessions is crucial.
Those with additional stressors such as life or personal stress, or managing a digestive health condition like IBS may be at more risk to develop this syndrome. I have seen a few athletes with IBS who have experienced overtraining syndrome in my practice.
What causes it and are you at risk? Overtraining syndrome is thought to be caused by systemic inflammation and subsequent effects on the central nervous system, including reduced mood, central fatigue, and neurohormonal changes. It can be hard to bounce back from and may take weeks or months.(3)
So when it comes to exercise – increased training loads are necessary for performance, but our rest and recovery are ESSENTIAL to ensure that our body will adapt to the physiological demands, rather than break down.
How Gut Health & IBS May Impact Recovery

There are a few ways that having IBS may impact your ability to recover well, and we will touch on them briefly.
Naturally, exercise can alter blood flow and functional capacity of the gastrointestinal (GI) tract leading to uncomfortable and debilitating side effects.(4) GI effects can happen before, during and after trainings and competitions.(4) Most at risk for GI disturbances are athletes competing in high intensity training like runners, triathletes, and cyclists. This is due to the intensity of the sport, as well as heightened risk for dehydration. Further, these athletes require taking in high concentrations of carbohydrates during training which can cause increased symptoms if not absorbed or tolerated well.
So for those with IBS, these experiences can be even more heightened and may lead some athletes to restrict their food, water and/or supplements around training events for fear of exacerbating their symptoms.
It’s important to remember that there are many things that we can control, and that IBS does not need to control your life and fitness goals. With the right strategies, you can help maximize your recovery and maintain the active lifestyle you want to have with IBS!
Key Nutrition Components for Recovery

Now that you’ve got the basics down, let’s review the key nutrition components that support the recovery process along with some IBS appropriate and low FODMAP examples.
Energy Balance
Energy balance occurs when our caloric intake (aka food intake) matches our energy expenditure output (5). Factors that increase our energy expenditure include training/exercise, environmental exposure (heat, cold, or altitude), fat-free mass (FFM), stress, illness, or some medications. FFM includes any non-adipose (aka fat) body weight such as bone and muscle, which are considered ‘metabolically active’ and therefore having higher bone and/or muscle mass means your resting metabolism will be higher.
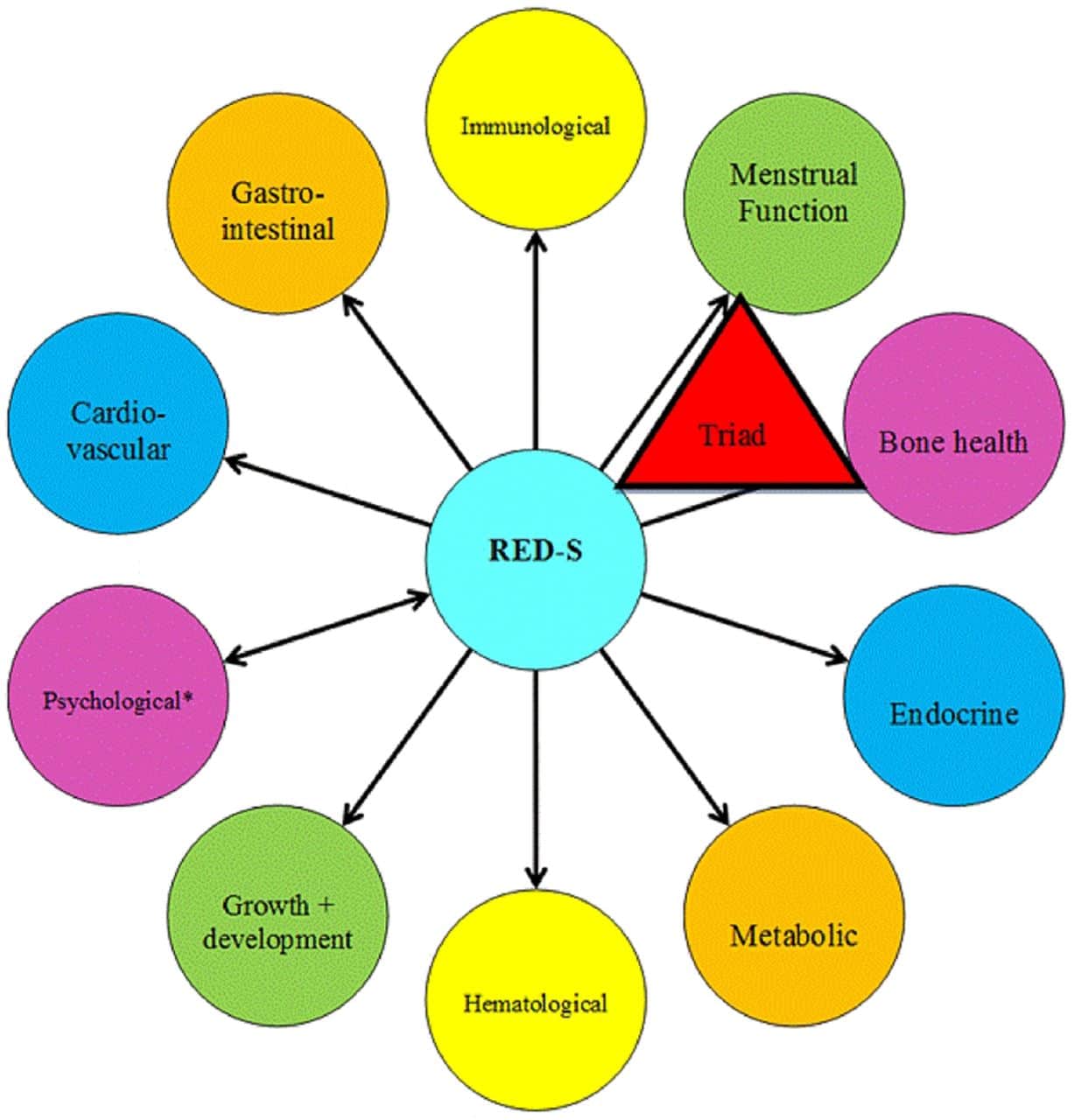
If we are chronically undereating to support your performance in relation to your energy expenditure, this can increase risk for Relative Energy Deficiency Syndrome (REDs). According to the International Olympics Committee, “The syndrome of RED-S refers to impaired physiological function including, but not limited to, metabolic rate, menstrual function, bone health, immunity, protein synthesis, cardiovascular health caused by relative energy deficiency.” (6)
Undereating can also worsen IBS symptoms, as blood sugar swings may contribute to changes in motility. It may also increase risk for binge eating and/or overeating which can also be associated with bloating and discomfort due to the volume of portions consumed.
Furthermore, IBS may be associated with low body weight due to symptoms inhibiting one’s desire to eat the caloric amount associated with their training demands.
Note: some athletes or active individuals may want, or be required, to lose or gain weight for their specific sport. Even if this is the case, meeting energy needs to support training is crucial. Work with a Registered Dietitian to help develop the right plan. Most often, IBS should be managed first and gut health restored, before a weight loss/ body composition plan is put into place.
Hydration

Did you know that dehydration can increase your perception of effort up to 30%? This means exercise can feel harder if you aren’t well hydrated! Furthermore, dehydration can increase risk of a gastrointestinal event/flare-up during or after high intensity exercise.
Being properly hydrated on a regular basis helps with:
- Maintaining healthy skin & joints
- Supports immune system
- Brain function (memory, mental clarity)
- Digesting food
- Removing wastes through blood, poop & urine!
Hydration Goal:
- Baseline: Drink 1L (32 oz) of fluids per every 50 pounds of your body weight daily.
- Plus ADD an additional 250-500ml (1-2 cups) every 30 mins of moderate to high intensity activity to your daily target.
Keep in mind fluids are not just water, you can include water, herbal teas (ginger, fennel, peppermint), milk, broths, and other non-caffeinated beverages in your daily target.
The above is just a guideline and you may have different needs based on a medical condition, increased losses, etc. Always speak to a Registered Dietitian and/or your Medical Doctor for guidance.
For low FODMAP beverages you can make at home check out our collection.
Protein

Protein is made up of amino acids which are the building blocks for muscles, bones, blood, hair, skin, nails, hormones, enzymes, chemicals. Pretty much everything in our body is made from protein!
We want to maintain a protein balance whereas the amount we take in either matches or slightly exceeds the amount we use. Too little protein on a regular basis can result in reduced recovery, impaired immune system, hormonal imbalance, cravings, hunger, and fatigue. Along with reduced recovery, this can lead to increased cravings, overeating and fatigue which can exacerbate IBS symptoms.
Please refer to the Monash University smartphone app and FODMAP Friendly smartphone app for the most up-to-date serving sizes of the following suggestions.
Protein Sources (low FODMAP):
- Animal: Chicken turkey, fish, shrimp, eggs, egg whites, lactose-free cottage cheese & greek yogurt, collagen protein powder
- Plants: tofu (firm), tempeh, edamame, quinoa or pea protein isolate powder
- Small amounts in hemp hearts, quinoa, nutritional yeast, chickpeas/lentils
Approximate Targets:
- Endurance Athletes: 1.4 – 1.6 g/ kg of body weight per day
- Strength Athletes: 1.5 – 2.0 g / kg of body weight per day
We want to divide this goal into 4-6 meals/snacks per day.
Keep in mind needs will vary based on age, medical conditions, injury, training status, etc. We would use adjusted body weight (AjBW) to calculate targets if your BMI >25 and high body fat %.
Carbohydrates
Carbs are the body’s primary energy source! They fuel our muscles and brain for activities of daily life, as well as exercise. Those who are active have higher carbohydrate needs.
However, those with IBS may fear carbs due to their presence of fiber and FODMAPs. Restricting carbs has not only negative consequences for exercise performance, but also the gut microbiome.
Active individuals and those with IBS should focus mainly on complex carbs at mealtimes that provide slow digesting energy as well as fiber, B vitamins and prebiotics.
Carbohydrate Sources (low FODMAP):
- Whole grains: quinoa, wild, black, red or brown rice, buckwheat, amaranth, millet, bulgur, farro, rolled or steel cut, oatmeal, quinoa/corn/rice pasta, sourdough bread.
- Starchy vegetables: sweet potato, potatoes, butternut squash, plantain, cassava, pickled beets
- Legumes: canned chickpeas and lentils, chickpea or lentil pasta, adzuki beans.
- Fruits: bananas (yellow), kiwi, blueberries, orange, pitted dates, etc.
Eat the Rainbow

How many colors do you eat each day? This is a great (and simple) way to ensure you are eating a diet that supports optimal gut health and performance! The natural pigments (aka colors) in fruits and vegetables have powerful antioxidant activity, meaning they help to fight off free radicals, prevent cell damage and reduce inflammation. (7) This is important for IBS and gut health, as there is often presence of chronic inflammation in the gut, however those who are more active have increased antioxidant needs as well.
Aim to include at least 2 colors with each meal. Some examples:
- Red: Red bell peppers; strawberries; raspberries
- Orange: Carrots, oranges, cantaloupe, pumpkin, rutabaga, sweet potatoes Yellow: Yellow bell peppers, pineapple, lemons, parsnips
- Green: Spinach, kale, zucchini, green beans, Swiss chard, collard greens, arugula, green bell peppers
- Purple: Eggplant, purple grapes, purple potatoes, red cabbage
- Blue: Blueberries
Nitrate Rich Foods
In both supplement and whole food form, nitrates are used to help support improved physical performance, in particular endurance and sprint type performance like running, cycling and swimming. (8)
By increasing the body’s circulating amount of ‘nitric oxide’, consuming nitrates helps improve the body’s oxygen carrying capacity – aka make workload easier. They can also help with soft tissue injuries (muscles, tendon, ligaments) by increasing blood flow.
Low FODMAP examples of nitrate-rich foods include (include at least 4-5 days/ week):
- Watercress
- Lettuce
- Spinach
- Celeriac
- Chinese Cabbage
- Endive
- Fennel
- Parsley
- Rhubarb
- Arugula
- Pickled Beets
- Swiss Chard
Supplements
While a food first approach is key, there are some supplements that may benefit athletes and those with IBS. In my practice I generally recommend these daily supplements:
- Multivitamin: A multivitamin and mineral supplement can be helpful to ensure covering nutrient bases for high performance athletes/ very active individuals, those with restricted diet (food intolerances, allergies) and/or excess losses/loose stool (IBS-D, IBD).
- Vitamin D: In the winter and fall months most of us cannot get enough vitamin D from the sun, supplementing is important to help immunity, mental health and mood (which is key for the gut-brain axis). It’s also a crucial nutrient to help support bone health and prevent stress fractures which are common in athletes.
- Magnesium: Many people following a low FODMAP diet tend to lack magnesium due to restrictions around quantities of plant foods. Not to mention, athletes have increased needs due to the demands of training. Magnesium is key for muscle contractions, sleep, and carbohydrate utilization so getting enough to meet your needs is crucial. Note: increase the dosage slowly as too much magnesium at once can increase bloating, loose stools and cramping due to its osmotic effect (ie. it draws water into the bowels).
- Protein powders: These can be helpful to help meet protein requirements with an active lifestyle and/or food restrictions. We have a guide on low FODMAP protein powders to help you choose the right one for you.
- Omega-3 (EPA & DHA): A good quality omega-3 supplement is one I often recommend to my active clients with IBS. It may be helpful if low fatty fish intake and/or vegetarian diet, high training levels, presence of anxiety, depression, ADHD, and/or inflammation present (IBS, recurrent injuries, GERD, joint pain). Take a plant-based source (typically made from algae) if you are vegan/vegetarian.
If you are an endurance athlete, carbohydrate products are important for fuelling. Check out our article: How To Fuel When You Have IBS: All About Low FODMAP Sport Gels, Sport Drinks & Snacks.
Please speak with your Registered Dietitian to find out which supplements and dosages are right for you and your needs!
This article will also be helpful: Medications & Supplements for IBS.
Additional Ways to Support Exercise Recovery & GI Health

Here are additional ways to support your optimum exercise recovery and gastrointestinal health.
Hot/Cold Therapy
Contrary to popular belief (and social media trends), ice baths post workout aren’t actually confirmed by strong evidence to bolster post-exercise inflammation and optimize recovery. Regardless, hot or cold therapy after workouts may help to prevent DOMS (delayed onset muscle soreness). (9)
There are benefits of cold therapy such as taking cold showers and ice baths related to mood and mental health. Cold water exposure has been shown to improve dopamine levels (8). While not studied directly in IBS and digestive health, we can speculate that engaging in cold water treatments may help digestive health through supporting the gut-brain axis.
Taking a hot bath can also be a great way to relax, which can help with regulating your nervous system which we know can help with digestive health and reducing IBS symptoms. Add some epsom salts which dissolve into magnesium and sulfate which may help reduce inflammation, lower stress, and decrease muscle soreness.
Massage
Massage is not shown to help directly improve sports performance, however it may help to reduce delayed onset muscle soreness (aka DOMs, muscle pain you feel 1 or 2 days AFTER a workout), improve relaxation and mood levels, all of which can help with the training process and digestive health. (10)
Full body massages are great, but consider trying out an abdominal massage in addition to your typical sports treatment. Those with chronic digestive conditions tend to hold a lot of tension in our core area, but focusing on these muscles may help reduce some of the tension and potentially improve digestive functioning. (11)
Sleep

Sleep is the pillar of health – without optimal sleep our body can’t function at its best. Sleep loss can impact exercise performance, as well as our digestive functioning (12). Experts recommend between 7-9 hours of sleep per night for adults (13). Athletes may need even more than this.
Some ways to support sleep include getting morning sunlight exposure to support melatonin production, keeping your bedroom cool, blocking out all light at night, and taking magnesium.
For further tips to improve your sleep, may want to read: How Does Sleep Impact IBS?
More Support
As always, reach out to a registered dietitian for support with fuelling your performance as well as managing IBS. Check out our Global Registered Dietitian Directory.
Ready to fuel your workouts and sports performance, while keeping IBS and gut symptoms at bay with the right tools and strategies? My Pre & Post Workout Nutrition For a Happy Gut: Mini Course & Resource Bundle might be the next step for you! Use code FODMAPEVERYDAY for 15% off the usual price.
The Takeaway
In the pursuit of fitness goals while managing IBS, understanding the intricate connection between exercise, recovery, and nutrition is so important. Maximizing recovery doesn’t just aid in performance, but also mitigates the risks of injury, digestive impacts, and keeps your motivation as an athlete high.

For those balancing active lifestyles with IBS, prioritizing recovery becomes even more crucial. As we’ve discussed, nutrition plays a vital role in supporting recovery by focusing on energy balance, hydration, protein, carbohydrates, and a colorful, diverse diet. Furthermore, looking at our lifestyle habits and utilizing additional treatments – sleep, hot/cold exposure, body work – we can further support the recovery process and GI health.
By working through these strategies, you can help to pave the way for good gut health alongside meeting your fitness milestones. This may be a lot to work through on your own, which is why we always recommend working with a Registered Dietitian.
Are you an athlete with IBS? We would LOVE for you to leave us a comment below and let us know what you took away from this article!
Summary:
- Recovery and Nutrition: Understanding the link between exercise, recovery, and nutrition is crucial for athletes managing IBS. Prioritizing recovery aids performance, reduces injury risks, and sustains motivation.
- Impact of Exercise on the Body: Exercise causes natural stress to the body, leading to physiological changes. Optimal nutrition facilitates the recovery process, helping the body adapt to exercise demands and get stronger overtime.
- Training vs. Working Out: Whether aiming for specific performance goals or exercising for health, maximizing recovery is pivotal for progress and keeping motivation high.
- The Importance of Recovery: Effective recovery ensures entering each training session at peak fitness, preventing illness, injury, and potential overtraining syndrome. Adequate rest, fluids, and refueling between sessions is as vital as increased training loads to see results.
- IBS and Recovery Challenges: IBS can heighten the impact of exercise-induced GI disturbances. However, with the right strategies in place, individuals can manage symptoms, maximize recovery, and maintain an active lifestyle.
- Nutritional Components for Recovery: Key factors like energy balance, hydration, protein intake, carbohydrates, and an antioxidant rich diet are pivotal for supporting recovery and gut health in individuals with IBS. Certain supplements including a daily multivitamin, Vitamin D, Magnesium and Omega-3 may also be helpful to address gaps in diet and/or meet increased needs.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1424733/#:~:text=Physical%20a ctivity%20in%20daily%20life,or%20maintenance%20of%20physical%20fitness.
- https://blog.nasm.org/the-science-of-recovery
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435910/
- https://www.abebooks.com/9781743073681/Clinical-Sports-Nutrition-Burke- Louise-1743073682/plp
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5753973/1
- https://bjsm.bmj.com/content/48/7/491
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8125642/#:~:text=Natural%20pi gments%2C%20including%20carotenoids%2C%20flavonoids,characterized%20b y%20powerful%20antioxidant%20activity.
- https://link.springer.com/article/10.1007/s00421-015-3166-0
- https://pubmed.ncbi.nlm.nih.gov/33493991/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10302181/
- https://pubmed.ncbi.nlm.nih.gov/33183670/
- https://pubmed.ncbi.nlm.nih.gov/35708888/
- https://www.nhlbi.nih.gov/health/sleep/how-much-sleep