As the population worldwide continues to live longer, approximately 14.5% of those living in the United States are categorized as older adults or over 65.1 There seems to be a lot of information available for adults living with digestive conditions, but we do not hear as much about the older adult population.

In my private practice, this population of older adults is looking for dietary help for improving digestion seems to be growing. Reviewing the current research, it is still unclear whether digestive problems in older adults are due to the normal aging process or a disease process.1
Underlying Causes of Digestive Problems in Seniors
This article aims to identify and discuss some potential underlying causes of digestive problems in older adults. Furthermore, this article discusses some of the most common digestive issues in older adults, including constipation, chronic diarrhea, gastroesophageal reflux disease (GERD), diverticular disease, and irritable bowel syndrome (IBS), as well as whether the low FODMAP diet can be of help.
Overview of the Digestive System
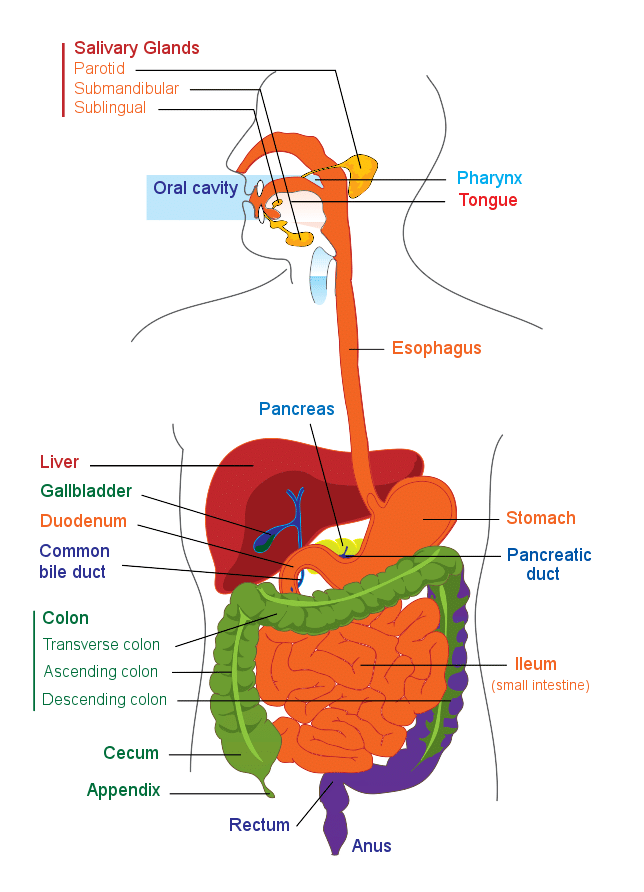
Before we discuss some of the reasons for digestive issues in older adults, here is a simplified overview of the digestive system.
The digestive system includes the GI tract and accessory organs, but this article will focus mainly on the oral cavity, esophagus, stomach, and small and large intestine in discussing the aging process.2 The purpose of the digestive system is to digest food, absorb nutrients, secrete enzymes, and eliminate waste products. Digestion sounds simple, but many things get off balance along the way.2
Oral Cavity Role in Digestion
The oral cavity plays a critical role in mechanically breaking down food in the chewing process and providing saliva and enzymes to help begin the process of breaking down carbohydrates and fats.2 Older adults often experience issues related to the oral cavity, including dry mouth, change in taste, burning mouth, and difficulty chewing due to ill-fitting dentures or other dental problems. Some of these issues might be related to medication side effects or a zinc deficiency related to poor dietary zinc intake.1
The Role of the Esophagus
Some older adults may also experience difficulty swallowing associated with a specific condition or from reduced motility in the esophagus. Swallowing problems can often impact the amount and types of foods a person can eat and thus may lead to nutritional deficiencies and even unintended weight loss.1
The Role of the Stomach in Digestion
Several changes in the stomach are commonly seen in aging that might impact the digestive process, leading to various digestive conditions. The most common include alterations in the gastric microbiota, a reduction in mucosal protection, reduced gastric blood flow, and slower gastric motility. Some of these changes could result from medication side effects, decreased activity levels, or related to conditions such as diabetes and Parkinson’s disease.1
You may want to read: Vital Organs: Stomach
Small Intestines and Digestion
Interestingly, the small intestine in older adults is not much different than in younger adults. However, small intestinal bacterial overgrowth (SIBO) is common in older adults, especially those hospitalized or living in a long-term care facility. SIBO is found in up to 15.6% of older adults and often includes symptoms such as chronic diarrhea, malabsorption, weight loss, and nutrient deficiencies due to high levels of bacteria in the small intestine.
It is usually caused by low stomach acid, poor motility, or medication side effects. The most common medication that can increase the risk of SIBO is proton pump inhibitors, which treat GERD.1 Poor motility is often blamed on the aging process, but surprisingly, it is not the effect of aging that slows things down, it is more often related to medications, polypharmacy, and other medical conditions, including diabetes.1
You may want to read: SIBO: Get the Facts
Large Intestines and Digestion
The large intestine is a common area of dysfunction in older adults struggling with chronic constipation. Most experts agree that motility is not the consequence of normal aging, and constipation is often the result of other factors that we will discuss in more detail later in this article.1
A final important area related to digestion is the gut microbiome. The gut microbiome is the biggest collection of microorganisms found in high numbers in the large intestine. Research has shown that the aging process, diet, and lifestyle factors impact the gut microbiome.3
The gut microbiome slowly evolves from birth until about the age of three, when it becomes more stable and diverse with healthy bacteria. Microbiome stability continues throughout most of a person’s adult years and becomes more unstable later in life. Although there is no ideal defined microbiome for older adults, typically less diversity of bacteria, shifts in some of the keystone species of bacteria, and increases in opportunistic bacteria are common patterns that might cause an imbalance overall. These changes in the gut microbiome might contribute to some of the digestive issues experienced in older adults.3
Diet and Lifestyle Factors
With a better understanding of how the aging process might impact different parts of the digestive system, dietary and lifestyle factors play a role. Medications and non-steroidal anti-inflammatory drugs (NSAID) may cause side effects that affect the digestive process and contribute to various conditions. Older adults may be managing multiple health conditions with more than five medications, also called polypharmacy, that can add to the complexity of digestive issues. As people age, they may also be less active and become sedentary, contributing to a slower digestive system, slower motility, and chronic constipation.4
Hydration
Hydration can be an issue for everyone, but it is especially challenging in older adults. Some physical changes happen as people age that cause a reduced sensation of thirst and a reduced ability to concentrate urine. These changes may cause older adults to be more prone to dehydration. Some older adults may experience a decline in cognitive function that causes them to forget to drink fluids during the day, have urinary incontinence that encourages them to self-restrict fluids, or poorly controlled diabetes that can impact hydration.
It might seem surprising how important hydration is to the body. It affects the skin, neurological function, kidney function, metabolic health, and gastrointestinal function. Dehydration is a common cause of constipation, although there are typically several factors that may be playing a role.5
Fiber
Low fiber intake is another factor that can impact the entire digestive system and lead to issues such as constipation. Fiber also reduces the risk of other GI issues, including hemorrhoids, diverticulitis, and colon cancer. In older adults, there can be physiological factors along with social and psychological ones that might impact the nutritional diet quality. Poor fiber intake can result from issues related to chewing that limit the ability to eat high-fiber foods, poor appetite that results in meals lacking in fiber, or even social isolation that can impact the amount and types of foods prepared for meals.6
You may want to read: Fiber and Irritable Bowel Syndrome (IBS): What You Need To Know
Common Digestive Issues in Older Adults
Diarrhea & Constipation
Constipation and chronic diarrhea are two conditions that are very common among older adults. Up to 30% of the general population struggles with constipation, and the elderly and women make up a large part of that statistic.4 Chronic diarrhea, on the other hand, affects about 5% of the population.7 The duration of symptoms, urgency or frequency of bowel movements, and the consistency of the bowel movements typically diagnose chronic diarrhea. Common causes of chronic diarrhea include irritable bowel syndrome, lactose intolerance, fat malabsorption, or poorly absorbed carbohydrates, such as fructose or sugar alcohol.7
Both constipation and chronic diarrhea can significantly impact a person’s quality of life and increase isolation for older adults. I often see this in my private practice when older adults avoid having meals with friends due to the fear of having an issue after dinner.
| Diet and Lifestyle Management of Constipation |
| Keep a routine that includes starting the day with light activity. |
| Gradually increase fluid intake to avoid dehydration while increasing fiber intake to around 25-30 g/day, depending on individual needs. |
| Increasing movement throughout the day to avoid a sedentary lifestyle. |

You may want to read: Strategies for Alleviating Constipation
GERD
GERD is another common condition that affects up to 23% of older adults. Not only is GERD the most common upper GI condition found in older adults, but it is often more severe and may lead to more complications than in younger adults.
Some of the common complications include esophagitis, Barrett’s esophagus, and esophageal cancer. Although many older adults experience less severe symptoms of GERD, the most common include heartburn and regurgitation. There are several underlying causes for GERD, including decreased saliva production, delayed gastric emptying, decreased pressure of the lower esophageal sphincter (LES), hiatal hernia, and reduced esophageal motility.
Lifestyle factors that can contribute to GERD are using tobacco, caffeine, and alcohol, consuming high amounts of fatty foods, being obese, and having a sedentary lifestyle. Addressing diet and lifestyle modifications can help reduce symptoms, but it is more common for doctors to take an aggressive approach to treating this condition due to the increased risk of severe complications. Treatment might include medications used either short or long-term.8
You may want to read: GERD, IBS & The Low FODMAP Diet
Diverticulitis
Diverticular disease is another prevalent GI condition found in older adults that increases in prevalence as a person ages. Approximately 70% of those over 80 are diagnosed with diverticulosis. Diverticula are small pockets that can form along the colon wall. Diverticulosis is when a person has diverticula but may or may not notice any symptoms. If the diverticula get inflamed, diverticulitis may occur, often including further treatment.9 The current recommendation for reducing the risk of diverticulitis is to have more fiber in the diet by adding more fruits, vegetables, whole grains, and legumes. Keeping body weight in a healthy BMI range and engaging in regular physical activity is also recommended.10
Irritable Bowel Syndrome
The last condition that can affect older adults is irritable bowel syndrome (IBS). The most common symptoms experienced with IBS include abdominal pain, gas and bloating, and altered bowel movements. IBS is more typically diagnosed in young adults and not commonly after age 65. IBS can be difficult to diagnose in older adults due to the similar symptoms in other conditions such as diverticular disease.
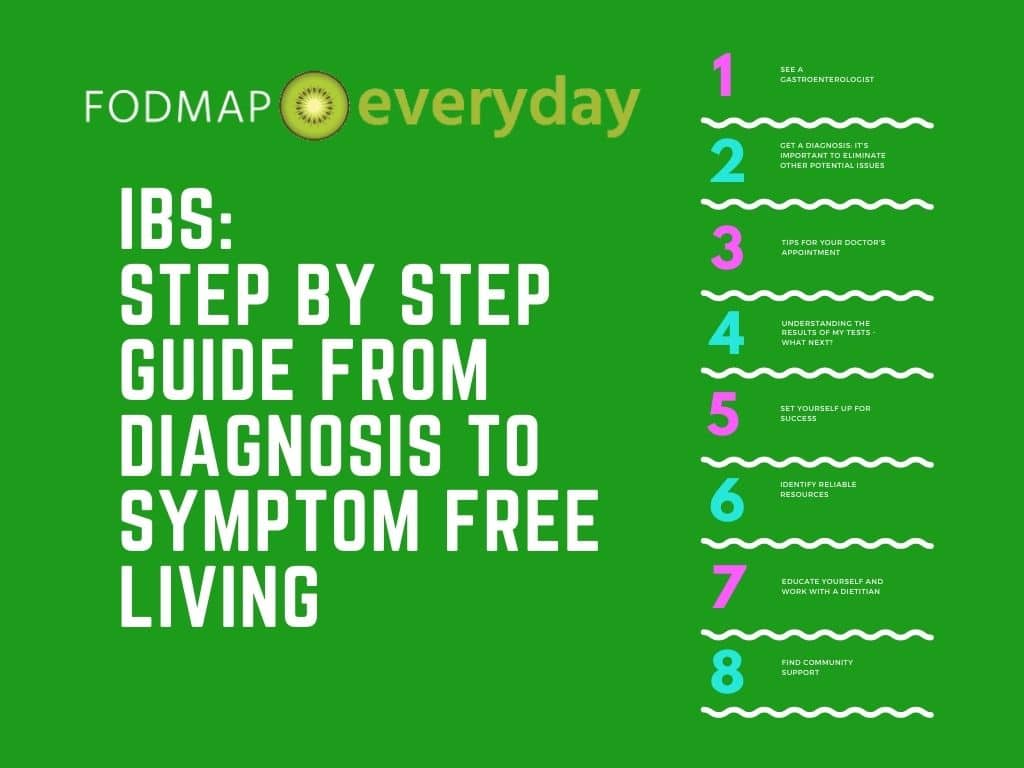
You may want to read: IBS: Step by Step Guide from Diagnosis to Symptom Free Living
Older adults may take multiple medications or NSAIDs that could lead to GI symptoms similar to IBS. A low FODMAP diet is one of the first-line dietary approaches for improving symptoms of IBS. A low FODMAP diet can help reduce the amount of fermentable fiber in the diet, along with helping to discover which types of FODMAPs are increasing symptoms.1
The Takeaway
Digestive health is critical throughout the life cycle, and some changes occur in the digestive tract as people age. Having a better understanding of the potential changes can make it easier to understand the symptoms or digestive conditions that might develop.
Many dietary and lifestyle factors play a role in preventing and treating digestive disorders, giving people more control over their health. The low FODMAP diet is an excellent example of a dietary approach that can help people manage IBS symptoms, making improving their quality of life easier.
References
1. Dumic I, Nordin T, Jecmenica M, Stojkovic Lalosevic M, Milosavljevic T, Milovanovic T. Gastrointestinal Tract Disorders in Older Age. Can J Gastroenterol Hepatol. 2019;2019:6757524. doi:10.1155/2019/6757524
2. Ogobuiro I, Gonzales J, Shumway KR, Tuma F. Physiology, Gastrointestinal. In: StatPearls. StatPearls Publishing; 2023. Accessed September 16, 2023. http://www.ncbi.nlm.nih.gov/books/NBK537103/
3. Salazar N, González S, Nogacka AM, et al. Microbiome: Effects of Ageing and Diet. Curr Issues Mol Biol. 2020;36:33-62. doi:10.21775/cimb.036.033
4. De Giorgio R, Ruggeri E, Stanghellini V, Eusebi LH, Bazzoli F, Chiarioni G. Chronic constipation in the elderly: a primer for the gastroenterologist. BMC Gastroenterol. 2015;15:130. doi:10.1186/s12876-015-0366-3
5. Li S, Xiao X, Zhang X. Hydration Status in Older Adults: Current Knowledge and Future Challenges. Nutrients. 2023;15(11):2609. doi:10.3390/nu15112609
6. da Silva GM, Durante EB, de Assumpcao D, de Azevedo Barros MB, Corona LP. High prevalence of inadequate dietary fiber consumption and associated factors in older adults: a population-based study. Rev Bras Epidemiol, 2019; 22: E190044. doi: 10.1590/1980-549720190044
7. Schiller LR, Pardi DS, Sellin JH. Chronic Diarrhea: Diagnosis and Management. Clinical Gastroenterology and Hepatology. 2017;15(2):182-193.e3. doi:10.1016/j.cgh.2016.07.028
8. Chait MM. Gastroesophageal reflux disease: Important considerations for the older patients. World J Gastrointest Endosc. 2010;2(12):388-396. doi:10.4253/wjge.v2.i12.388
9. Feuerstein JD, Falchuk KR. Diverticulosis and Diverticulitis. Mayo Clinic Proceedings. 2016;91(8):1094-1104. doi:10.1016/j.mayocp.2016.03.012
10. Bailey J, Dattani S, Jennings A. Diverticular Disease: Rapid Evidence Review. afp. 2022;106(2):150-156.







