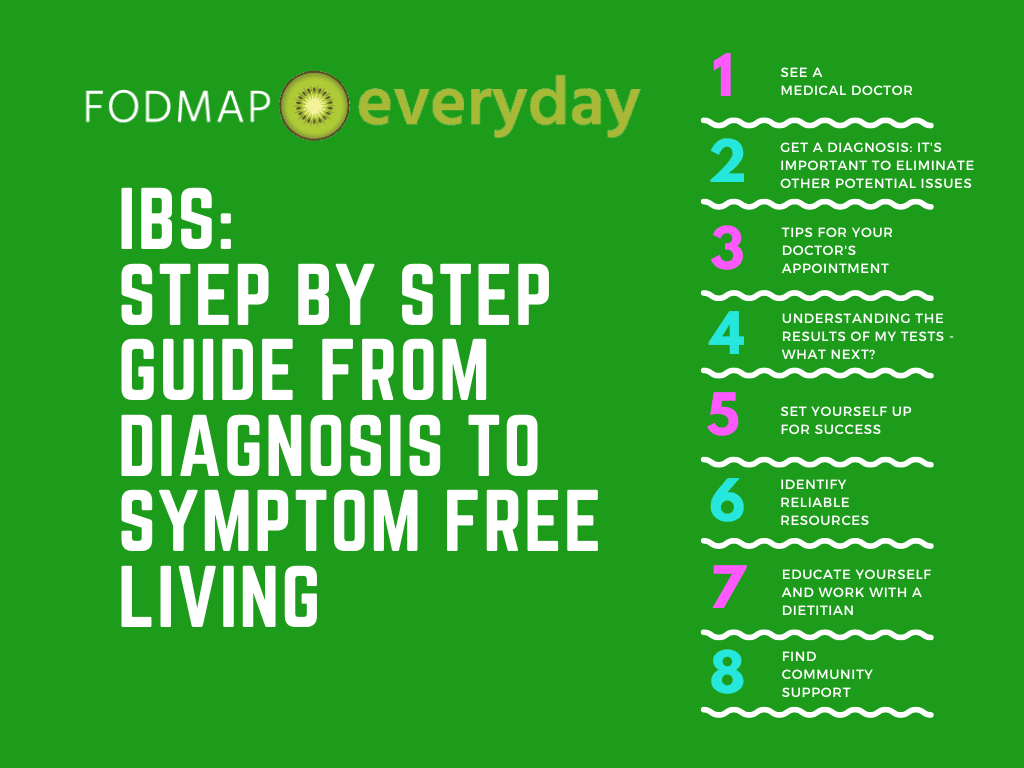
How do you know if you have IBS (Irritable Bowel Syndrome)? If recommended, how do you know if the low FODMAP diet is appropriate for you? And how do you make sure that you are following the low FODMAP diet the best way possible?
- What is IBS?
- How Do You Know If You Have IBS?
- Step 1: See A General Practitioner or Gastroenterologist
- Step 2: Getting a Diagnosis
- Step 3: Tips For Your Medical Appointment
- Step 4. Understanding the Results of My Tests: Now What?
- Step 5. Set Yourself Up For Success
- Step 6. Identify Reliable Resources & Tools
- Step 7. Educate Yourself & Work With A Dietitian
- Registered Dietitians To The Rescue
- Step 8. Find Community Support
- The Takeaway
This article is a step-by-step guide that will take you through all these questions one at a time. First, let’s define what IBS is.
What is IBS?
An estimated 10 to 15 percent of the worldwide population suffers from IBS (irritable bowel syndrome), a chronic digestive disorder of the large intestine that causes abdominal pain, diarrhea, constipation, or alternating episodes of both.
These symptoms are the result of abnormal intestinal motility –– too fast leads to diarrhea, too slow to constipation –– and increased sensitivity to pain. Bloating, gassiness, bowel urgency, and mucus in the stool are also common in IBS.
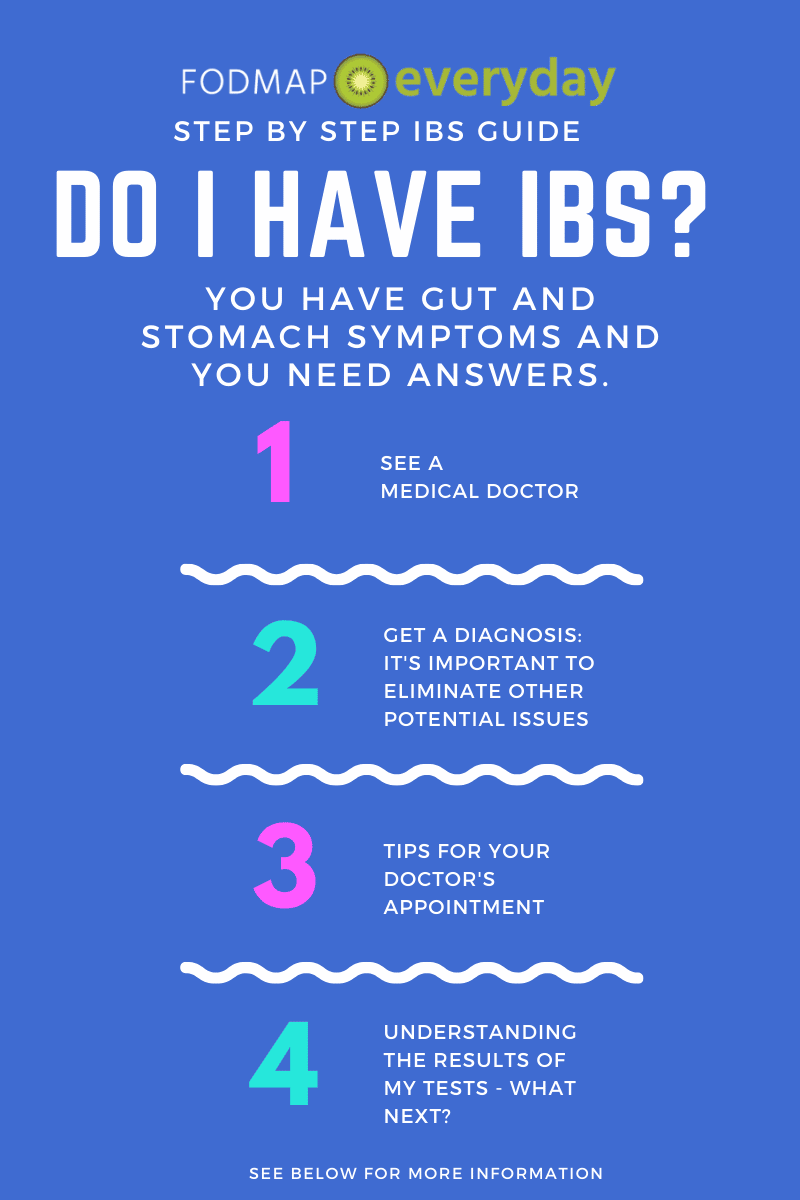
How Do You Know If You Have IBS?
There is no formal test for IBS that is widely used or particularly reliable*; IBS is typically diagnosed based on symptoms, after certain tests may be done which screen for diseases and conditions that present same or similar symptoms. It is also very important that you do not self-diagnose. We have provided you with easy-to-follow steps, outlined below, to help determine if you do have IBS.
*(Though there is no universally applicable diagnostic tool for all IBS forms, there is a relatively new, commercially-available antibody blood test called IBS-Smart. This test measures biomarkers associated with IBS-D and IBS-M, which may be elevated following infectious gastroenteritis and presents a potential diagnostic option for post-infectious IBS-D and IBS-M. As always, consult with your trusted health professional to learn more if they believe this may be a useful tool in your diagnosis Please read our previously published article that discusses this test for more information, and discuss the advantages and limitations with your medical team.)
Step 1: See A General Practitioner or Gastroenterologist
This is an essential step. We encourage you to see a medical doctor for a formal diagnosis.
The medical doctor that you see should be trained to review all the details of your medical history and symptoms, consider differential diagnoses, and perform any necessary testing to rule out other potential issues before issuing an IBS diagnosis.
General Practitioner vs. Gastroenterologist
Depending on your insurance, and where you live in the world, you might receive a diagnosis by your General Practitioner (GP), have to see your GP first to get a referral to a Gastroenterologist (GI), or be able to make an appointment directly with a GI. In the US our team recommends seeing a Gastroenterologist for the most accurate IBS diagnosis.
To find a gastroenterologist, you may reach out to your primary care physician’s office (GP’s office) for a list of in-network providers and a referral. You may also consider using the following resources:
Gastroenterologist Directories
- United States
- Canada
- UK
- Australia
- EU – search by country
- Latin America – search by country
- Asia/SE Asia- search by country
- India
If you do not live in a country with universal healthcare and cannot afford a GP or GI visit at present, there are some additional options to consider, such as free clinics. Most countries have universal health care; in the United States this is not currently the case, so take full advantage of the free clinic resources listed here and these additional suggestions:
- USA Free Clinic Directory
- Charity options at local hospitals
- Cash discounts (ask your doctor’s office)
Step 2: Getting a Diagnosis
There is no specific test for IBS; it is diagnosed largely based on symptoms once other conditions are excluded. Do not self-diagnose or use home test kits, as many medical issues (some very serious) can present with similar symptoms.
Your medical doctor should first review your full medical history and perform a physical exam, then will most likely order blood, urine and/or stool tests and screen you for celiac disease disease and other “red flag” symptoms that may need further investigation before a diagnosis of IBS can be settled on. Depending on your symptoms, they might also screen you for IBD (inflammatory bowel disease), Crohn’s Disease, diverticulitis and/ or endometriosis.
A colonoscopy might be recommended, and some doctors will order X-rays or CT scans, lactose-intolerance tests and/or breath tests for SIBO. It’s important to note that not everyone needs these tests for an IBS diagnosis, and your doctor is the best one to decide if they are indicated in your situation.
The Rome IV Criteria (the Rome Foundation creates guidelines for diagnosing IBS) is the gold standard for medical doctors to diagnose IBS. This can be implemented by a GP or a GI, although depending on where you are located, you may find some doctors more familiar with this than others.
A formal IBS diagnosis will be given when other medical issues are ruled out and your symptoms match those that are indicative of IBS, such as those presented in the Rome IV criteria.
A formal IBS diagnosis will be given when other medical issues are ruled out and your symptoms match those that are indicative of IBS, such as those presented in the Rome IV criteria.
Gut Microbial Composition
Recent scientific studies have shown that certain types of microbes are found in the gut of those who are more likely to have IBS; for instance, gammaproteobacteria seem to be in greater abundance in both children and adults who have IBS. Other pathogens, such as Clostridioides difficile, may also be contributing to IBS symptoms. Researchers are hopeful that these findings will aid in diagnostic and therapeutic approaches. In the future it might be possible to make very specific recommendations for individuals, for probiotics and prebiotics for instance, based on their unique gut microbe presentation.
The low FODMAP diet is one such approach that can alter microbial composition in a positive way for some of us with IBS.
Links for Further Reading
- National Institutes of Health: National Institute of Diabetes and Digestive and Kidney Diseases: Diagnosis of Irritable Bowel Syndrome
- Monash University: Diagnosis of IBS, Tests, and Investigations
- American College of Gastroenterology: IBS Screener
- The Rome Foundation
- Gut Micribiota For Health
Step 3: Tips For Your Medical Appointment
Getting in to see your gastroenterologist or doctor can sometimes involve a long wait for a brief appointment. That’s why, when your appointment comes, it is critical to have your symptoms and concerns clearly laid out. This will help both you and your doctor make the most of your visit.
First, your doctor will review your medical history and the purpose of your visit. To prep for this, it is helpful to have clear notes, or even printed documentation, that outline your symptoms (most doctors will love this).
Some details to include would be:
- Key symptoms of concern (i.e., bloating, constipation, diarrhea, alternating bowel habits)
- Symptom onset (i.e., when you started to notice the issue)
- Frequency of symptoms (i.e., daily, weekly, etc.)
- Location of symptoms (i.e., bloating above or below belly button, etc.)
- Severity of symptoms (i.e., scale or 1 to 10, how is it impacting your daily life)
- Timing of symptoms (i.e., middle of the night, after a meal, after a period of fasting, etc.)
- Duration of symptoms (i.e., last for 2 hours post-meal, etc.)
- Management strategies attempted to date (i.e., MiraLAX, fiber adjustments, etc.)
- Recent unexpected weight changes
- Recent diet adjustments
- Stooling Habits
- Consistency (using the Bristol Stool Chart)
- Frequency of bowel movements per week
- Presence of blood, mucus, oil (greasy looking stool)
- Color (gray, black, red, yellow; note that what you eat may impact stool color)
- Presence of straining to pass a bowel movement
Here is a simple symptom tracker; you may want to use to write down your symptoms over time.
Advocate For Yourself
After you share your current symptoms with your doctor, ask them if there are any symptoms that they would like you to keep an eye on and report back about during your next visit; this will help your care team identify any unexpected changes and adjust your care plan accordingly.
Next, you will want to outline 2-3 key questions you would like to address during your visit. Starting with the ones that are the most important to you and make your way down the list. These will vary person-to-person, but may include questions like:
- Are there any red flag symptoms in my history that warrant further testing? If so, which tests and why?
- Do you suspect IBS, and if so, why IBS and not something else?
- Do you think I might benefit from a referral to: a Gynecologist, Registered Dietitian (RD), Pelvic Floor Therapist, Gut-Directed Hypnotherapist?
- If I do require additional testing, what can I do between now and my labs/tests to manage symptoms?
Lastly, we suggest bringing a friend or family member with you to your appointment, who can take notes while you are talking with your doctor. COVID (or other) restrictions might not allow this as an option, though you may also ask if you can record the conversation on your phone, so that you can listen again afterwards and stay focused during the appointment.
Step 4. Understanding the Results of My Tests: Now What?
As we mentioned earlier, IBS diagnosis is based upon symptoms and excluding other medical issues. If your tests come back indicating that there are no structural issues underlying your symptoms, you may get news of an IBS diagnosis. Then you might be wondering: what caused my IBS?
It’s very frustrating to hear that the cause, much less the cure, for such a common condition remains unknown, but we do have more ways of treating IBS than ever before. These interventions generally fall into three categories: dietary, pharmaceutical, and psychological.
Dietary
The premier dietary approach for IBS –– the low FODMAP diet –– has been shown to provide significant symptom relief in as many as 75% of people who try it. That’s a remarkable statistic. It’s also why our goal at FODMAP Everyday® is to help you understand and incorporate the low FODMAP diet into your everyday life. You can read more about the diet here, and then start putting it into practice with our delicious low FODMAP diet recipes.
Please note that statistically and anecdotally you will have a far greater chance of success following the diet if you work with a Registered Dietitian (RD, also referred to as RDN), or equivalent in your country. We have a Global Dietitians Directory for you. These days many dietitians will offer remote sessions via Zoom, Skype or phone. This means RDs are more accessible than ever. Please read our article, Patient Dos and Don’ts for A Great Telehealth Appointment. Working with a RD can be the most helpful and impactful decision that you make. We cannot overstate how important we think it is to work with a RD.
Pharmaceutical
Medications for IBS are numerous but they often target only one of the predominant symptoms, which is problematic if you suffer from two or more. Other drawbacks to using drugs for IBS are the potential for side effects and cost.
Psychological
The most well researched psychological interventions for IBS particularly helpful for people whose symptoms are exacerbated by stress. Both Cognitive behavioral therapy (CBT) and gut-directed hypnosis have success rates that surpass many medications, but they also require a greater time and emotional commitment.
Follow The Treatment Plan: Be A Good Patient
These three points above are the broad strokes. There are non-medical tips and tools that can be employed as well, which we detail below. The crucial point is that your doctor will have laid out a treatment plan for you. It is vital that you understand what the recommendations are, and that you understand how to follow them. There are steps to take to learn how to maximize the results you get from following the plan.
The statements above might seem obvious, but we see people all the time not following the low FODMAP diet correctly or deciding to take a supplement because it was suggested on social media, without consulting their doctor or RD, to give two common examples.
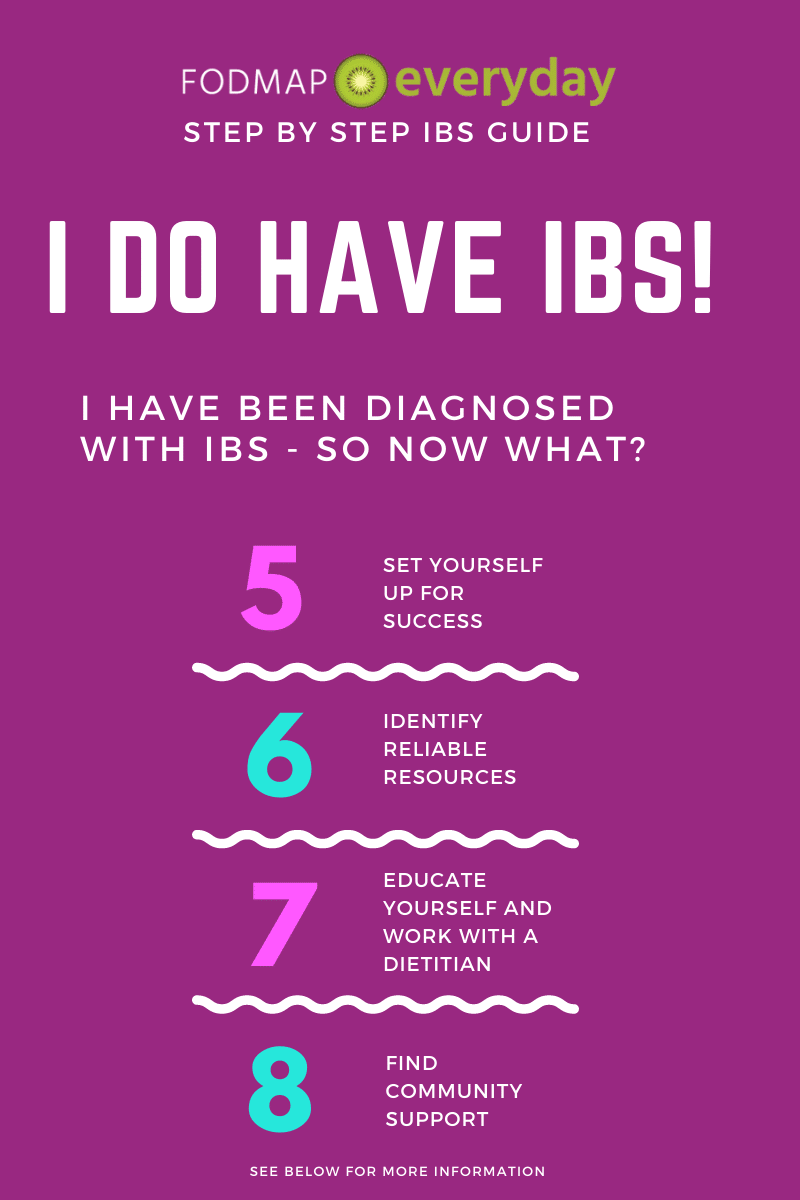
Step 5. Set Yourself Up For Success
The number one way to set yourself up for success in alleviating your IBS symptoms is to work with a Registered Dietitian, or the equivalent in your country – preferably one who is FODMAP savvy.
This is because RDs will be able to help you structure the right way for you to follow the low FODMAP diet (if that was suggested) – it is not the same for everyone – while also keeping track of, and consulting with you on, medications, supplements, triggers, symptoms, non-FODMAP related sensitivities as well as taking into account any other medical or lifestyle issues you might have. There is a lot to keep track of and learn about; your RD will be your team leader and help you at every turn.
In addition, we suggest extending yourself and your body and mind some compassion. As best you can, avoid falling into the mental trap that IBS is your “fault”, or that flares are a direct result of something that you’ve done. Focus on the habits within your control and establish a simple, repeatable plan to help you live joyfully and symptom-free!
A successful IBS care plan typically involves a holistic routine. In addition to potential dietary changes and possible medications or supplements, it might involve stress management techniques, sleep quality improvement, supportive mealtime and stooling habits, and a trusty toolkit (see below) in the event of a flare-up.
Here are some foundational habits to consider integrating into your day-to-day IBS care – this section is about addressing stress, anxiety, lifestyle choices and environmental impediments to success:
- Diaphragmatic breathing or “deep belly breathing” before meals. This technique stimulates the vagus nerve, which is like the nervous system superhighway that connects the brain and the gut. When the vagus nerve is stimulated through deep belly breathing, it tells the gut that it’s time to prepare for digestion by stimulating the autonomic (or “rest and digest”) nervous system. It also provides the immediate benefit of relaxing gastrointestinal muscles, which can help ease the experience of abdominal pain, bloating, constipation, and urgency. This can also be helpful during bathroom trips.
This YouTube Video is a great way to learn!
- Using a Squatty Potty, or similar tool, for more easeful defecation. Tools like the Squatty Potty allow your knees to elevate about 30 degrees above hip height while you’re seated on the toilet. This squatted positioning allows the puborectalis muscle to relax more readily, which helps with the final passage of stool without straining.
- Checking the menu prior to dining out to make sure you can identify some IBS-friendly options for yourself! This article is a helpful place to start.

You may want to read: How to Navigate a Restaurant Menu on the Low FODMAP Diet
- Mindfully chewing foods to applesauce consistency. The size of food particles when they arrive at your stomach and intestines makes a big difference on your comfort during the digestive process! The more you chew, the less work your gut and gut microbes need to do to breakdown food before absorbing nutrients. We speak to this at length in our Kitchen Yoga article.
- Low-impact movement and stretching. Compared to higher impact activities like interval training and running, low impact movement provides the benefit of stimulating movement along the gastrointestinal tract without the additional spike of cortisol, a stress hormone. Be sure to read through our 7 article IBS and Yoga Series.
You May Want To Read: IBS & Yoga Series
- Minimizing carbonated beverages and straw use. If bloating is a major symptom that you struggle with, limiting the amount of gas and air you swallow through things like bubbly drinks and straws is a helpful place to start.
- Abdominal massage. Not only is abdominal massage a relaxing way to soothe the muscles surrounding your small and large bowel, but it can also help to moderate gas pain and stimulate bowel movements for those with constipation.
Neurosomatic Massage Therapist Jenny Sprung teaches you essential self massage techniques in this YouTube video.
- Staying well-hydrated. This one is probably obvious, but the most obvious ones tend to be the easiest to overlook! Your level of hydration has a direct impact on your ability to easily pass stool without straining. It’s equally important to focus on hydration if you struggle with frequent diarrhea and are losing water and minerals through loose stools. Water is always good, with or without a squeeze of citrus for flavor, and we have many recipes for low FODMAP iced teas as well.
The IBS Flare Toolkit
In addition to the day-to-day basics, you may also consider building up an IBS flare toolkit. Everyone’s will look different depending on the symptoms you struggle with most, but some options are:
- A heating pad to soothe cramping and abdominal pain
- Enteric-coated peppermint capsules (like IBGard) to support abdominal comfort
- Loperamide (or Imodium) for those with IBS-D
- Senokot tables (or another laxative) for those with IBS-C
- Simethicone (or Gas-X) for trapped gas
Of course, if medication is part of the care plan suggested by your doctor, that would be an integral component of your routine as well.
Reading about other’s experiences can be helpful. We have an article for you on IBS attacks and also one on how our community members handle these flare-ups.
But please always remember, listen to your doctor and RD; follow their advice. Do not make any changes to your treatment plan without consulting them first.
Step 6. Identify Reliable Resources & Tools
We strongly suggest that you educate yourself about IBS, the low FODMAP diet and about any of the other recommendations that your doctor has made. The truth is that many doctors are not well-versed in the low FODMAP diet – which is also why working with a RD is so important. And the better educated you are, the more prepared you will be to work with your RD and help yourself get better, which is the goal!
Managing IBS requires that you have access to trusted, evidence-based sources to guide your care. Unfortunately, when it comes to the low FODMAP diet, there is a lot of misinformation out there; just because something says it is low FODMAP does not mean that it is. We see misleading high/low FODMAP lists, recipes and articles all the time.
Here below is a guide to resources we do recommend:
General IBS & Low FODMAP Resources
These are our top go-to websites that provide information on IBS, the low FODMAP diet and related issues:
- American College of Gastroenterology: IBS Resources
- International Foundation for Gastrointestinal Disorders
- Monash University
- FODMAP Friendly
- FODMAP Everyday® – of course. We have hundreds of articles for you written by Monash University trained RDs.
- GI Institute
Monash University & FODMAP Friendly
Monash University and FODMAP Friendly get their own shoutout. These are the only two entities that are performing lab testing for FODMAP content and are considered primary resources. If the low FODMAP diet is part of your treatment plan, you should spend time getting acquainted with both. When in doubt, refer to these resources.
FODMAP Everyday® is accredited by FODMAP Friendly as an educational FODMAP resource, and our Success Team RDs are Monash University trained, as is our lead recipe developer, Dédé Wilson, who is also FODMAP Friendly accredited.
There’s An App for That!: Smartphone Apps for Managing IBS
There are many smartphone apps that can bring a world of help to the palm of your hand.
For Tracking Symptoms:
- Bowelle App: Mood, food and symptom diary app – available in the App Store for iPhone
- Cara Care: IBS symptom tracker iPhone and Android
Gut Directed Hypnotherapy App
- Nerva: Nerva is an app-based IBS hypnotherapy program that can help retrain your gut-brain link. Available for iPhone and Android. Learn more about Nerva here. Try Nerva For Free! And get 20% off after the 7-day free trial with our special discount offer for FODMAP Everyday® readers! Just click below.
Low FODMAP Diet Resource and Management Apps
- Monash University Smartphone App: Use to learn FODMAP levels and quantities in foods, search for low FODMAP certified products, track your intake with the built-in food diary, access recipes, and read additional resources from the Monash team.
- FODMAP Friendly Smartphone App: Use to learn the FODMAP content of foods, appropriate serving sizes, view their list of low FODMAP certified foods, and have access to videos, recipes, meal plans and more. Their app was completely overhauled in early 2022 and you can read more here.
- Real Plans: The Real Plans meal planner is a low FODMAP meal planning, shopping, and cooking tool. It includes FODMAP Everyday® recipes within a robust tech system that allows you to plan meals, snacks, incorporate leftovers, create shopping lists taking your pantry items into account, and many more features. You can set it to your exact specifications. For example, you can search for low FODMAP recipes that are vegetarian, never include mushrooms, and teach the system that you always have olive oil on hand, so there is no need to add it to grocery list. Streamline your low FODMAP shopping and cooking!
Shopping Apps
- Spoonful: This is a barcode scanner app that allows you to scan products in your grocery story and get instant information on the potential FODMAP content in that product. You can also filter for vegan, vegetarian and pescatarian (more diets being added). They also offer “swap” information and have a shopping list function. The scanned information is derived from product labels, not from actual lab testing. Please use in conjunction with the Monash University app. Learn about the Spoonful App here!
- FIG (“food is good”): This is a scanner app that allows you to filter for FODMAP content of prepared foods in addition to dairy-free, corn allergies, fructose intolerance and more. The information is based on product labels, not from actual lab testing, but it is all reviewed by Monash trained dietitians. Please use in conjunction with the Monash University app. You can read our interview with the developers here.
Books
There are many books available, including one by our own FODMAP Everyday® co-founder, Dédé Wilson. Please keep in mind that books will contain information that was up to date at the time of publication.
- The Low FODMAP Diet Step-by-Step by Dédé Wilson & Kate Scarlata RDN LDN
- The 28-Day Plan for IBS Relief: 100 Simple Low-FODMAP Recipes to Soothe Symptoms of Irritable Bowel Syndrome by Audrey Inouye BSc RD & Lauren Renlund BASc MPH RD
- The Bloated Belly Whisperer by Tamara Duker Freuman MS RD CDN
- The Gut-Friendly Cookbook: Delicious Low-FODMAP, Gluten-Free, Allergy-Friendly Recipes for a Happy Tummy by Alana Scott
- The Complete Low-FODMAP Diet: A Revolutionary Plan for Managing IBS and Other Digestive Disorders by Sue Shepherd PhD and Peter Gibson MD
- The Low-FODMAP IBS Solution Plan & Cookbook by Rachel Pauls MD
And many others we share here!
Step 7. Educate Yourself & Work With A Dietitian
Since the low FODMAP diet is the primary dietary recommendation made by gastroenterologists if you have an IBS diagnosis – and since you are here at FODMAP Everyday® – we assume you want to learn about the low FODMAP diet.
There are many ways to educate yourself about it, such as via the resources mentioned above, but keep in mind that a recent study found that IBS patients who worked with a dietitian during implementation of the low FODMAP diet had a better overall understanding of the protocol and symptom response compared to those who did not. And, most importantly, this translates to experiencing more success with the diet, meaning symptom relief.
So, if your doctor does recommend that you trial the low FODMAP diet, it is highly recommended that you ask them for a referral to a FODMAP-trained Registered Dietitian, or peruse the directories listed here to find the right dietitian for you:
- FODMAP Everyday® Global Registered Dietitian Directory
- Monash University IBS Dietitian Directory
- International Foundation for Gastrointestinal Disorders Dietitian Directory
Registered Dietitians To The Rescue
The low FODMAP diet is meant to be undertaken along with a Registered Dietitian (RD, or equivalent in your country). The diet is nuanced and complex; statistically and anecdotally you will have a greater chance of success if you work with one.
We have put together a series of articles that discuss working with a dietitian to help you learn why you should work with a dietitian, how to find the right dietitian for you, the difference between dietitians and nutritionists, what to expect from working with one, tips for successful telehealth appointments, and more.
Please take the time to familiarize yourself with these articles and resources:
- Have IBS? Top Reasons To Work With A Dietitian
- How To Choose A Dietitian
- Dietitians & Nutritionists: What’s The Difference?
- Patient Dos And Don’ts For A Great Telehealth Appointment
- What If The Low FODMAP Diet Isn’t Working?
Outside of FODMAPs, your dietitian will also help to ensure nutritional adequacy of your diet and assess other variables, like fiber balance, hydration status, non-FODMAP food triggers, and non-food triggers for your IBS.
Take This Course!
If you’d like to learn more about IBS independently, there is also a fabulous course offered through Monash University called the Monash FODMAP and IBS Training for Patients. This course provides a step-by-step guide to manage IBS symptoms using the low FODMAP diet.
Buy Certified Low FODMAP Products
Lastly, while you’re getting accustomed to your low FODMAP protocol, you can explore some of the fabulous certified low FODMAP products, spices, and meals available for FODMAPers these days. Many of these trusted producers also share resources on their websites that may be useful to you.
Some include:
For all the certified low FODMAP brands be sure to regularly visit the websites of Monash University and FODMAP Friendly. You may also want to follow Monash and FODMAP Friendly on Facebook to keep up to date on all of the latest information about certified brands and research.
Step 8. Find Community Support
Chronic and otherwise “invisible” conditions like IBS can feel both frustrating and isolating at times. This is one of the many reasons why joining a community where IBS, symptoms, management strategies, and recipe sharing can be a huge help to folks living with the condition. You’ll see firsthand that you’re not alone and have a place to go to when you need an ear!
We just caution you that social media is not the place to seek a diagnosis, or to discuss your individual medical issues. That should be overseen by your medical team, who know you personally. The groups listed have been vetted by our team, with the exception of Reddit. We have included it because it has a very active, vibrant FODMAP community. We just caution you that responses may come from someone who has really studied the science, or someone who is not well educated in the science. It is usually not possible to know what the credentials are of anyone responding or posting. Always do your due diligence. We think the best groups are clearly moderated by FODMAP trained experts who rely on evidence-based information.
General IBS Patient Support Groups
- IBS Patient Support Group
- IBS Support (respected evidence-based Facebook group with almost 90K followers)
- UK Based IBS Network
- Canada IBS Support Group (Canada specific Facebook group)
The FODMAP Everyday® team recognizes the importance of community in IBS care, and for that reason, we’ve worked hard to cultivate several spaces where you can join us to connect!
- Facebook FODMAP Everyday Page
- Facebook Low FODMAP for FOODIES Group
- Facebook Uncensored Low FODMAP Recipes
- Instagram FODMAP Everyday Community
- Pinterest FODMAP Everyday Community
The Takeaway
IBS is a very common gut-brain disorder than can be diagnosed by a gastroenterologist after other medical conditions, that present similarly, are excluded. Do not self-diagnose.
There are steps you can take before your appointment to be prepared. Keeping a symptom diary for a couple of weeks beforehand can help you formulate your questions as well as provide the doctor with specific information, unique to you. This can aid in your diagnosis as well as provide information that might inform what recommendations are made for you going forward.
The low FODMAP diet is the premier dietary approach for IBS and has been clinically proven to provide significant symptom relief in as many as 75% of those following the diet; it will very likely be recommended by your GI, if you receive an IBS diagnosis. Certain pharmaceutical and psychological options might be proposed as well.
There are also many non-medical tools and tactics that you can employ to help yourself, such as creating an IBS toolkit, learning abdominal massage and breathing techniques, practicing mindful eating, and more. Certain books, websites and social media groups can be helpful as well – but always vet the source. Who is running the Facebook group? Who wrote that book? What are their credentials?
A FODMAP trained dietitian can make sure that you are following the diet correctly, are addressing any concurrent issues (diabetes, weight management, vegetarian diet, etc.) and that you end up with a positive relationship with food in the end – all while addressing your IBS triggers and making sure that you remain nutritionally sound. You have a much greater chance of becoming pain-free if you work with a dietitian. Set yourself up for success.
Learn what resources are evidence-based and reliable. Monash University and FODMAP Friendly are the two entities that are performing lab testing for FODMAP content and are considered primary resources. Download both of their smartphone apps ASAP; these provide the easiest access to the most up-to-date accurate FODMAP information. FODMAP Everyday® is accredited by FODMAP Friendly as an educational FODMAP resource, and our Success Team RDs are Monash University trained, as is our lead recipe developer, Dédé Wilson, who is also FODMAP Friendly accredited.
Take advantage of our Real Plans meal planner and of lab tested and certified low FODMAP products made by companies like Belliwelli, ModifyHealth, Gourmend Foods and many others. You can find all of these certified foods in the Monash University and FODMAP Friendly apps.
There is no one reason why someone develops IBS and there is no cure. What a doctor and dietitian can do is provide an accurate diagnosis and a plan to minimize or eliminate most of your IBS symptoms. FODMAP Everyday® is here to help you learn to thrive on the low FODMAP diet while living with IBS.