Diseases of the pancreas can mimic other medical conditions, and accurate diagnosis is crucial.
With the increase in access to information through social media it is becoming more and more common to hear about individuals who were incorrectly diagnosed (or self-diagnose), only to find out later that it was a more serious condition.
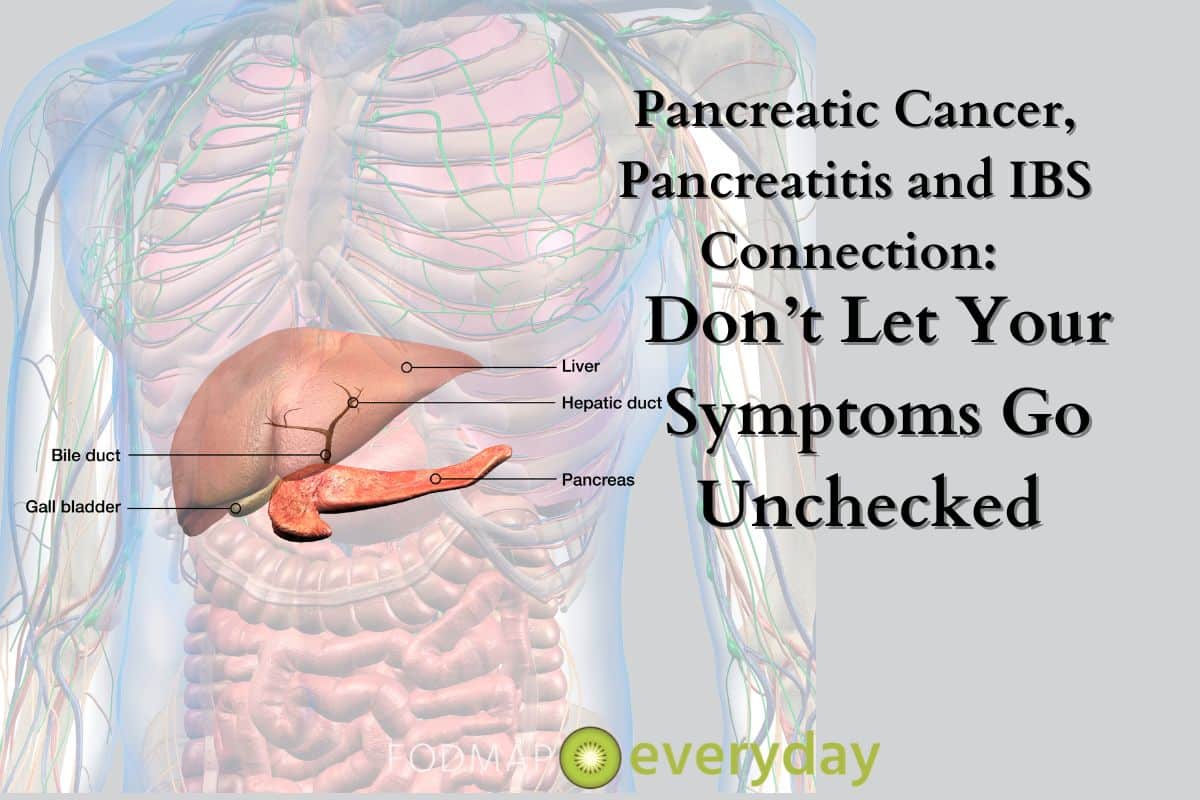
Certain diseases share symptoms with irritable bowel syndrome (IBS), some of them potentially deadly if left undiagnosed or treated. It is important that you are seen by a competent gastroenterologist who has reviewed your medical history, current symptoms, and has undertaken the necessary tests to rule out more serious conditions.
Overlap of IBS Type Symptoms with Pancreatic Disease
It is known that there is a large overlap in symptoms that occur in disease of the pancreas and Irritable Bowel Syndrome (IBS). Conditions including, but not limited to, endometriosis, diverticulitis and Crohn’s are considered ‘differential diagnoses’ for IBS. Misdiagnosis of any of these conditions may occur before the proper diagnosis is made.
Diseases of the pancreas can be very serious if left untreated, and thus a proper diagnosis is essential. In this article, we will highlight common pancreatic diseases, including pancreatic cancer and pancreatitis, and the symptoms that occur that may overlap with IBS, to help spread awareness of these significant but commonly misdiagnosed conditions.
While IBS is a true diagnosis, if you are experiencing any of the additionally noted abnormal symptoms, press your doctor for adequate testing and thorough investigation to rule out differential diagnoses.
For those of you experiencing pancreatitis, we will also present general guidance to support this condition and your pancreatic health through nutrition.
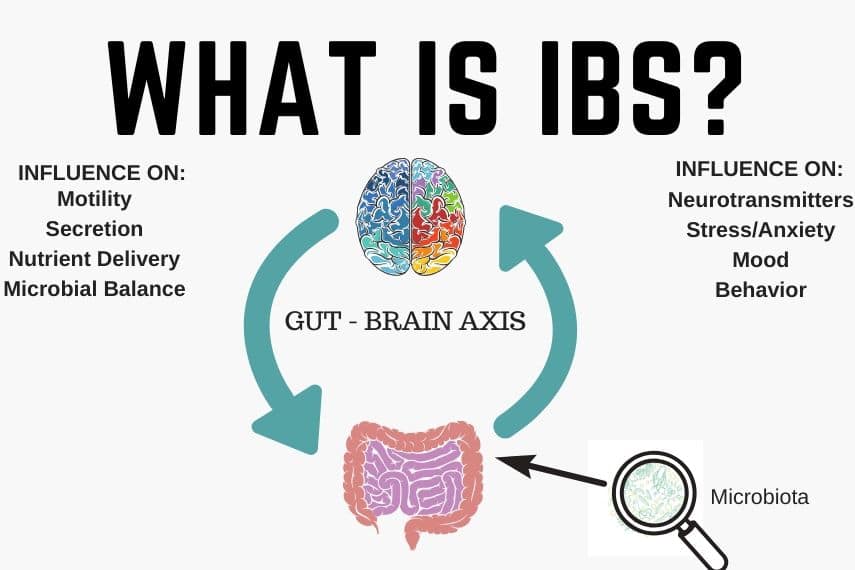
What is IBS?
You probably already know what IBS is, but let’s do a quick recap to help highlight the similarities between IBS and pancreatic diseases.
IBS is a chronic, functional gut disorder characterized by abdominal pain or discomfort along with a range of other symptoms, including bloating, diarrhea, constipation, or alternating episodes of both. If you have IBS, you know it can be a debilitating condition with a variety of symptoms that impact your quality of life as well as your physical and mental health when not managed properly.
The main/primary symptoms of IBS include:
- Abdominal pain, cramping and/or discomfort
- Constipation (inadequate and/or infrequent bowel movements)
- Diarrhea (loose, unformed stool)
- Bloating (sensation of an inflated balloon in your abdomen)
- Distension (visible increase in abdominal girth/size)
Other symptoms those with IBS may also experience:
- Flatulence/excessive wind
- Urgency with bowel movements
- Fatigue/ low energy
- Nausea
- Reflux and/or heartburn
- Bowel incontinence (not being able to make it to the bathroom in time)
- Anxiety, depression
Although the exact cause of IBS is not known, it is thought to have some underlying symptom drivers including dysbiosis, visceral hypersensitivity, dysmotility, altered gut-brain connection, and chronic low grade inflammation in the gut.
For a deeper dive, we suggest reading What is IBS?
What is the Pancreas? A Small But Mighty Organ
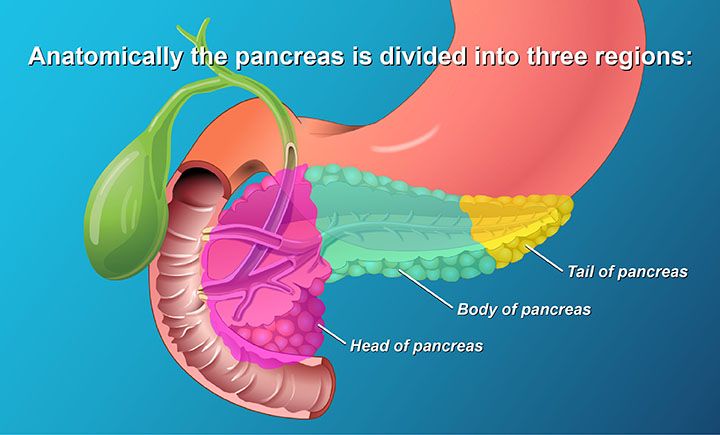
Most people don’t know where this organ is, or what it does for us. The pancreas plays a critical role in our digestive functions, as well as regulating energy and metabolic health.
The pancreas is a flattened gland that is about 6-inches in size, which is roughly the length of a US dollar note or two baseballs side to side. It’s sandwiched between your stomach and your spine (1).
It may be small, but our pancreas is a mighty organ with some very important roles. When we consume food, our pancreas secretes enzymes that help us to break down food including:
- Lipase: Breaks down fats (ie. the primary macronutrient oils, nuts, seeds, fatty fish)
- Protease: Breaks down proteins (ie. the primary macronutrient in meats, eggs, tofu)
- Amylase: Breaks down carbohydrates (ie. the primary macronutrient in grains, fruits, starchy vegetables)
It also plays an important role in creating hormones that are released into the bloodstream which impact our metabolic health as well as digestion, including (2):
- Insulin: Insulin is the hormone that helps sugar enter your cells. Without insulin, sugar builds up in the blood and overtime this leads to Diabetes.
- Glucagon: When blood sugar gets too low (ie. when we are hungry or exercising), glucagon is released which sends a message to the liver to release stored sugar.
- Gastrin: Some gastrin is made in the pancreas which plays a role in making stomach acid which we need to break down food like proteins.
- Amylin: Amylin is also produced by the pancreas and helps regulate appetite and stomach emptying.
Now you know what the pancreas is and how it relates to your health. We hope you won’t take it for granted (any longer).
Diseases of the Pancreas
Now that we understand the role of the pancreas, let’s discuss what happens when the pancreas is not well with an explanation of three of the most common pancreatic diseases.
Pancreatitis
Pancreatitis, as the name sounds (itis = inflammation), is inflammation and swelling of the pancreas. It occurs when digestive juices or enzymes attack the pancreas. There are two general forms of pancreatitis including (3):
- Acute: Short term inflammation that may subside and the pancreas returns to normal.
- Chronic: Long lasting inflammation that may come and go. It leads to long term damage and scarring of the pancreas, and may even impact its ability to produce insulin (the hormone that helps bring sugar from our blood into our cells) which can result in diabetes.
Pancreatitis may be caused for various reasons including certain medications, alcohol abuse, infection, high triglyceride levels, cystic fibrosis, tumor or trauma to the pancreas (ie. such as a motor vehicle accident or sports injury) (3).
Symptoms of pancreatitis may include (3):
- Extreme abdominal pain, and may spread to your back
- Nausea, vomiting
- Fast heart rate
- Fever
- Fluid accumulation in the upper belly
- Sore/tender upper abdomen
- Low blood pressure
- Yellowing of the skin and eyes (ie. jaundice)
- Diarrhea/oily stools
As you can see, some of these symptoms also occur in IBS such as stomach swelling (which can be mistaken for bloating/ water retention as a result of sub-optimal digestion), loose stools and abdominal pain.
Pancreatic Cancer
Pancreatic cancer is a type of cancer that starts in the pancreas. Cancer occurs when cancer cells grow out of control and outgrow normal cells (4).
Pancreatic cancer does not show any symptoms until it has progressed. The main symptoms include (4):
- Nausea and vomiting
- Low appetite
- Diabetes (rare, but can occur if the cancer damages the pancreatic cells)
- Jaundice including darkened urine, light coloured stools, greasy stools, and itchy yellow skin (if cancer has spread to the liver)
- Enlarged gallbladder or liver
- Belly/stomach or back pain
- If you experience any of the above symptoms you should contact your medical doctor immediately and not wait for them to pass or continue.
Diabetes
As mentioned above, the pancreas is where our hormones that regulate blood sugar including insulin and glucagon are produced. So, if something is wrong with the pancreas (ie. inflammation, swelling, scarring) this can result in abnormal levels of these hormones produced. If insulin is not being properly released, this would result in sugar building up in the blood and lead to diabetes.
In Type 1 diabetes, often referred to as “early onset diabetes”, the pancreas attacks its own healthy cells and it can no longer make insulin.
With Type 2 diabetes, often referred to as “adult” or “lifestyle” diabetes, either cells become resistant to insulin (usually in early stages of diabetes and prediabetes) and eventually the pancreas may give up and stop producing insulin after producing excess trying to compensate (often in the later stages of diabetes).
There is a connection between IBS, our gut microbiome, and insulin sensitivity. If you are interested in learning more, you may want to read: IBS & Diabetes: The Connection & How to Eat If You Have Both.
If you are interested in learning more, you may want to read: IBS & Diabetes: The Connection & How to Eat If You Have Both.
Pancreatic Diseases & IBS: Risks of Misdiagnosis
Pancreatitis & IBS
As you can see above, abdominal pain and many of the other symptoms like diarrhea and swelling of the abdomen in pancreatitis could easily be mistaken for IBS. In a study, IBS-like syndrome was determined in 54 (63.5%) patients with prolonged (more than 4 weeks) exacerbation of chronic pancreatitis (5). This gives us indication that chronic pancreatitis can cause symptoms that are very similar to IBS, and result in misdiagnosis, although it is not clear on the prevalence of this.
Whether mild or severe, pancreatitis most often requires hospitalization to ensure it does not progress. If you are experiencing severe abdominal pain, nausea, or vomiting that isn’t getting better, don’t try to “tough it out”. Seek medical advice to rule out anything serious.
While we aren’t trying to scare you into thinking any of your flare-ups may be something more serious, this is just a reminder that sometimes there can be more serious concerns going on and if you suspect something is not right, seek help.
Pancreatic Cancer & IBS
Pancreatic cancer, sadly, can also sometimes be misdiagnosed or assumed as simply being IBS in its earlier stages. Misdiagnosis of cancer can result in delayed treatment times and increased risk of finding the cancer in its later stages when the cancer has progressed and potentially spread to other organs. Pancreatic Cancer Action has a section on their site on how to identify common pancreatic symptoms and advocate for yourself with your medical team if you suspect your symptoms may be more than IBS: Common Misdiagnosis of Pancreatic Cancer.
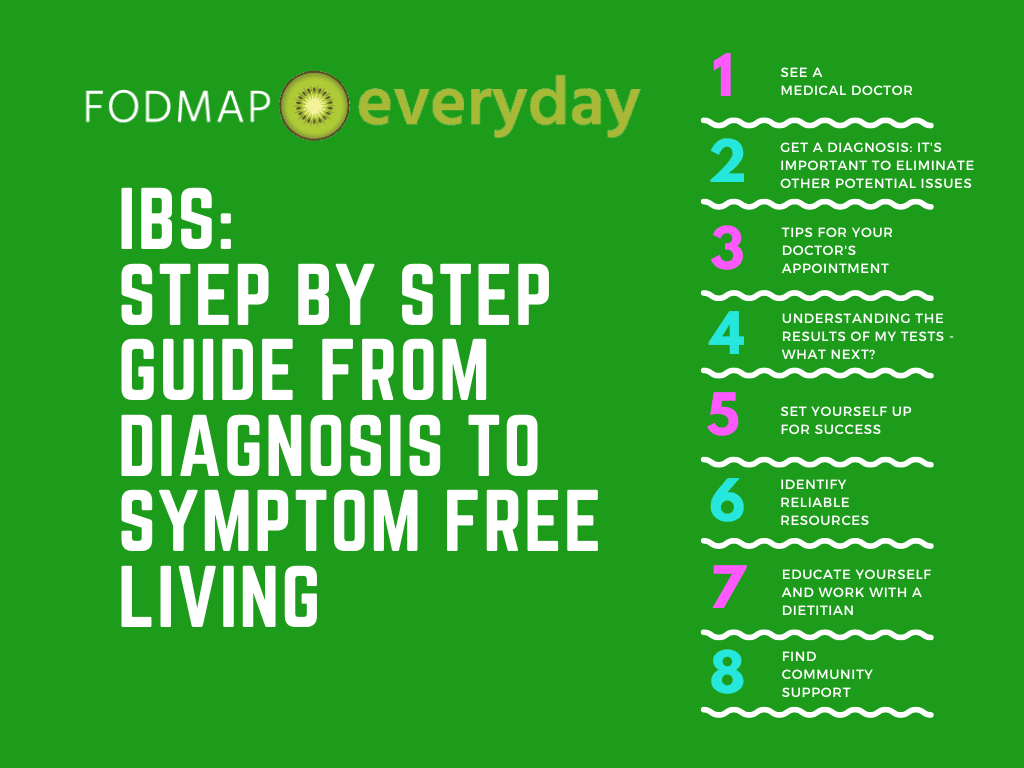
Our take home message for you today is that if you “suspect” you might have IBS based on your symptoms, but have not received a diagnosis from a medical doctor, we highly encourage you to seek one! Always discuss your symptoms with your general practitioner (GP) and ask for investigations to confirm an IBS diagnosis and rule out differential diagnoses.
If you do not feel you are receiving adequate care from your medical team, consider a second or even third opinion. As we mentioned above, some people assume that it is “only IBS” and let more life-threatening conditions like pancreatic (or colon cancer for that matter) go unchecked which may have devastating consequences.
You might want to read this article: Take Back Control: How to Identify and Tackle Medical Gaslighting.
Nutrition For Pancreatitis
While not the main focus of our article, let’s discuss some general strategies to support pancreatitis and related digestive function if you experience this condition.
If you have acute pancreatitis, you will likely be advised by your medical team to stop eating and may be placed on IV fluids. As you recover, you will likely transition to a low fat, low fiber diet, and then if symptoms improve, slowly return to a regular diet.
With chronic pancreatitis, it will depend on the severity of your symptoms and have different long term needs. Although the damage with chronic pancreatitis is not completely reversible, it is thought that with long term dietary changes you can help your pancreas function as best it can. Some strategies that may be recommended include (6):
- Eating smaller frequent meals: 5-6 times per day is recommended to help reduce the portion that your digestive system is breaking down in a sitting.
- Lower fat diet: Not a “no fat” diet (we need fat for energy, hormones, etc.) but a lower fat diet is recommended. This means limiting/avoiding foods like fried foods, creamy sauces, skins on meats, fatty meats like sausage and bacon.
- Fiber intake: Whole fruits, vegetables, grains and pulses are important for a diet that supports pancreatic health long term as they are high in fiber, prebiotics and antioxidants which can help regulate inflammation and support digestive function.
- Supplementation: Those with chronic pancreatitis are at higher risk for malnutrition (ie. nutrient deficiencies) due to issues with absorption, especially fat soluble vitamins like A, D, E and K. Oftentimes a multivitamin is recommended as well as extra care to ensure supplementation of any suspected deficiencies.
Pancreatitis, just like IBS, is difficult to manage on its own, which is why we always recommend consulting a Registered Dietitian. You may want to read our series of articles on Working With A Registered Dietitian.
The Takeaway
To conclude, the overlap of symptoms of pancreatic diseases, such as pancreatitis and pancreatic cancer, and IBS underscores the importance of seeking proper medical examination. Self-diagnosis, misdiagnosis, or delayed diagnoses, can have severe consequences, as highlighted by instances where symptoms thought to be IBS were actually related to pancreatic cancer.
If you have been given a diagnosis of IBS, but you have persistent, worsening or additional symptoms, we encourage you to advocate for testing and investigation with your medical team and/or ask for a second or third opinion if needed. Further, as IBS and pancreatic diseases can be difficult to manage, we suggest building your care team with the right practitioners including a Registered Dietitian.
Summary
- The pancreas plays an important role in digestion as well as hormone regulation. Damage and/or disease in the pancreas can lead to digestive difficulties, blood sugar issues, nutrient deficiencies and more.
- Pancreatic diseases like pancreatitis and pancreatic cancer often show symptoms similar to Irritable Bowel Syndrome (IBS), such as abdominal pain and changes in bowel habits, which may lead to misdiagnosis or delayed diagnosis.
- Seeking accurate medical diagnosis for your condition is crucial, as these conditions require distinct treatments and may have severe consequences if left untreated.
- Nutrition for chronic pancreatitis includes smaller frequent meals, tailored supplementation, lower fat diet and a diet rich in plant foods.
References:
- Pancreas Foundation https://pancreasfoundation.org/pancreas-disease/
- Hopkins Medicine https://www.hopkinsmedicine.org/health/conditions-and-diseases/the-digestive-process-what-is-the-role-of-your-pancreas-in-digestion
- Hopkins Medicine https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatitis#:~:text=points%20about%20pancreatitis-,Pancreatitis%20is%20the%20redness%20and%20swelling%20(inflammation)%20of%20the%20pancreas,pancreas%20and%20let%20it%20heal.
- Cancer.org https://www.cancer.org/cancer/understanding-cancer/what-is-cancer.html
- PubMed https://pubmed.ncbi.nlm.nih.gov/32598720/
- My Health https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=abk6873