Have you ever felt like your Irritable Bowel Syndrome (IBS) symptoms are all just “in your head”? The bloating, pain gas… Sometimes it seems too painful to even be real.

Perhaps you were diagnosed with IBS by your general practitioner (GP) or gastroenterologist (GI), but you feel like you weren’t given enough investigation, and there could be more going on to explain your symptoms.
Or maybe you’ve had TONS of tests done because you feel like there are more answers to your symptoms, including SIBO breath testing and motility tests, that all come back normal. But you are still experiencing painful bloating – so what does that mean?
Well, to be absolutely clear here: IBS is a true medical condition and your symptoms are valid! It is one of the most common gastrointestinal disorders and is characterized by alterations in bowel habits, as well as recurring abdominal pain, bloating, and/or gas. IBS is considered a ‘functional gut disorder’ meaning that there are no underlying mechanical or structural abnormalities that would explain your symptoms.
While we don’t know the exact cause, IBS symptoms are thought to be exacerbated by a few factors including motility changes in the small and large intestines, altered gut-brain connection, dysbiosis in the gut microbiome, post-infectious reactivity, and visceral hypersensitivity in the intestines (6).
Visceral hypersensitivity is considered to be one of the keystone factors in the development of irritable bowel syndrome symptoms, like abdominal pain and bloating (12).
So while you may wonder if your painful symptoms are just “all in your head”, this article is intended to discuss the connection between IBS and visceral sensitivity and help you gain a better understanding of what is going on in your body and brain, and the connection to the symptoms you experience!
What Is Visceral Hypersensitivity?
Visceral hypersensitivity refers to altered or heightened sensations in response to physiological stimuli (6).
Pressure or volume changes in the bowel would be examples of stimuli: such as larger food portions, or fermentation (aka gas) from food consumed.

Essentially visceral hypersensitivity means that your tolerance or threshold for pain in your intestinal lumen is lower, so even the normal functioning of your intestinal organs and digestion of food can feel painful (12).
Approximately 40% of people with IBS are thought to also experience visceral hypersensitivity.
Getting into the science a little bit (for those of you that like the details), the two major components of visceral hypersensitivity include: (6):
- Hyperalgesia: an increased pain sensation in response to a stimulus which usually provokes pain. It would be normal to experience pain in the situation, but the pain response is heightened. For example, feeling intense, excruciating pain to a sunburn that would usually cause pain, but be manageable in nature.
- Allodynia: an elevated/enhanced nociceptive (aka perception of) pain sensation in response to normal stimuli (aka a pain response to a stimulus which does not usually cause pain). For example: a light feather touch could cause someone extreme pain (7).
Not surprisingly, visceral hypersensitivity is considered a common driver for symptoms in functional disorders like IBS as well as functional dyspepsia (aka indigestion), dysmenorrhea (aka menstrual pain) and fibromyalgia (aka chronic pain and fatigue syndrome). Although the exact connection and overlap is not yet clear, approximately 40% of people with IBS are thought to also experience visceral hypersensitivity (15).
It should be noted that visceral hypersensitivity is now being considered a medical diagnosis on its own, and is diagnosed by a healthcare provider through applying small amounts of internal pressure to certain organs (15). For women this can often be experienced during yearly gynecological exams when the medical practitioner does external palpating.

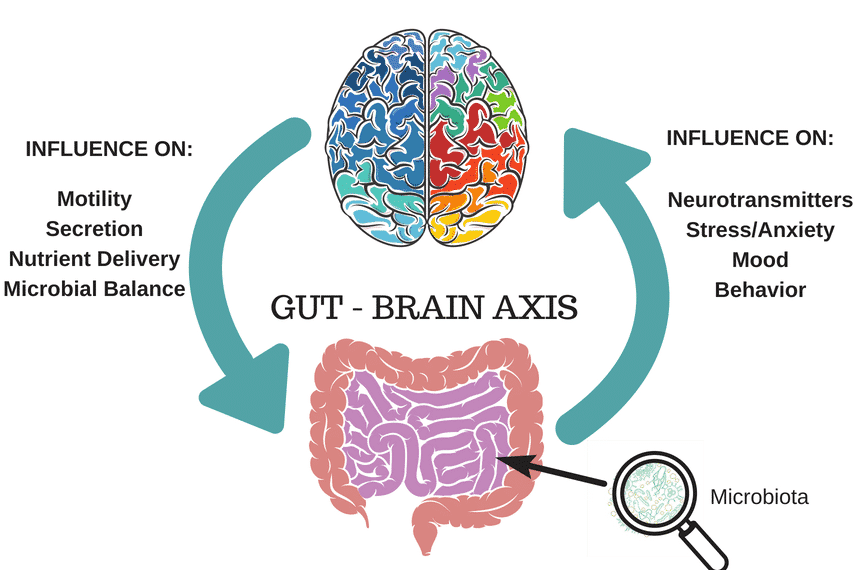
IBS, the Gut-Brain Connection & Visceral Hypersensitivity
As mentioned, IBS is considered a “functional gut disorder”, meaning that there are no known structural issues to explain symptoms, but there does seem to be some dysfunction between our gut and brain communication.
Fascinatingly, our digestive system actually has its own nervous system and this is why it is known as the “second brain”. Our gut contains many nerve endings and receptors that are influenced by hormones, gut bacteria, digestive components and the stretching and movement of our gut (pretty cool!) (15).
Our digestive system actually has its own nervous system and this is why it is known as the “second brain”…When we have visceral hypersensitivity in our intestinal organs, these receptors have altered tolerance to pain during normal digestion, and so these messages are sent to our brain and cause the intensified discomfort we feel.
When we have visceral hypersensitivity in our intestinal organs, these receptors have altered tolerance to pain during normal digestion, and so these messages are sent to our brain and cause the intensified discomfort we feel.
As you know if you have IBS, it can feel quite debilitating and it is hard for those who do not experience IBS to relate to the pain you may experience. It can also seem like a mystery to you that eating a hamburger and fries can send you into a full blown IBS flare-up for 2 weeks, while your good friend can suffer no consequences! Well, your decreased tolerance to pain after consuming potential irritants to the gut can be explained by visceral hypersensitivity.
Some examples of factors that could cause someone with IBS increased pain levels could include:
- Carbonated/fizzy beverages (due to introducing additional air into the intestinal tract)
- Large portion sizes (increased volume can cause intestinal pain by stretching the intestinal walls)
- Fatty, fried foods (due to their high fat content can slow motility and emptying)
- High FODMAP foods (aka highly fermentable foods, that cause increased gas in the bowels can trigger sensations of pain)
So while sometimes it might feel like it’s “all in your head”, to some extent it might be when considering the gut-brain connection and heightened pain response (aka visceral hypersensitivity) in IBS. However, that doesn’t mean that there isn’t anything you can do about it, or that your symptoms are not valid. By understanding how nerves in our gut and our gut-brain connection impact our symptoms, we can better manage our symptoms by addressing this connection (more on that below).
There is also a large overlap between IBS and endometriosis, and visceral hypersensitivity is considered a common symptom driver in both conditions (5). So if you also have endometriosis, for example, you also know the debilitating pain with your menstrual cycle, likely caused by visceral hypersensitivity in your uterus and reproductive organs.
You May Want To Read: The Gut-Brain Connection & IBS: It’s Not All in Your Head
What Causes Visceral Hypersensitivity?
My guess is you don’t just want to just settle with an understanding of what visceral hypersensitivity is, you’re keen to know what can cause it, and how to get to the bottom of it!
While the research is new and ongoing, we do have some underlying theories of causes and contributing factors to visceral hypersensitivity including:
Gut Microbiome
Changes in the gut microbiome and dysbiosis are becoming more recognized as a driver for symptoms and the development of IBS. People with IBS are recognized as having an imbalance of “good” and “bad” microbes in their gut (fungi, bacteria, methanogens, etc.).
This could be due to gastric infections, high stress levels, poor diet, post-pregnancy, celiac disease or other risk factors contributing to an imbalance in the gut microbiome. Certain types of pathogen bacteria can trigger visceral hypersensitivity in IBS by degrading the strength of the intestinal wall and lead to what is known as “leaky gut syndrome” which may exacerbate visceral hypersensitivity (12).
You May Want To Read: The Microbiome Explained
“Leaky Gut Syndrome”
As mentioned above, “leaky gut syndrome” or more technically known as “increased intestinal permeability” is characterized by small holes in the intestinal wall and a weakened gut barrier which can allow bacteria and toxins to leak into the bloodstream (4). There is some controversy around leaky gut as there is no exact way of diagnosing it yet, but there is though that it may be linked to gut dysbiosis as well as an increase in mast cells associated with IBS (18).
You May Want To Read: What Is Leaky Gut Syndrome?
Mast Cells
Mast cells, which are types of white blood cell that are responsible for immediate allergic reactions located all over your body, may contribute to the development of visceral hypersensitivity and IBS (3). Increased number of mast cells (ie. above normal amounts) can contribute to increased gut permeability (weakening of the intestinal barrier), which increases visceral hypersensitivity. Some factors that may increase mast cells include gastric infection, food allergies, increased fatigue and increased psychological stress levels (11,3).
You May Want To Read: COVID-19 & IBS: “Long COVID”, Mast Cell Activation & Histamine Intolerance
Genetics
Our genetics play an important role in our body’sies physiology. Having a relative with a functional gut disorder, or mental health condition, could predispose us to visceral hypersensitivity and increased pain responses. With that said, our environment can “flip the switch” to turn genes on or off, so the other factors discussed here would play a role in whether or not these genes would be expressed.
Early Life Trauma & Adverse Childhood Experiences
Adverse childhood experiences (ACEs) and early life trauma have been associated with decreased pain tolerance, as well as increased risk for anxiety and depression in adulthood. As the brain is still growing and changing in childhood, experiencing ongoing neglect, stress and/or abuse can lead to a shift in how one’s brain cells are wired due to constantly being in a fight or flight situation (8,9).
Psychological Disorders
Did you know that people with IBS have a threefold risk of anxiety and depression (13)? The same mechanisms that contribute to visceral hypersensitivity can lead to anxiety and depression. With that said, people with these conditions may constantly be activating stress circuits thereby increasing pain sensitivity.
How Can You Improve Pain Tolerance in Visceral Hypersensitivity?
When it comes to improving pain tolerance in visceral hypersensitivity, the research is still growing. However, considering what we know about its causes and triggers, we can extrapolate on some strategies to help address these factors.
There are two main considerations for strategies to help improve visceral sensitivity: one is a long term approach to help improve your pain threshold, and the other is to help reduce the triggers that are causing you increased pain.
Improve Pain Threshold
Gut-Brain Support
Improving the gut-brain connection is considered an impactful adjunctive strategy to manage symptoms in IBS by helping improve pain tolerance and regulate the communication between our gut and brain. Some ways to help improve your gut brain include:
- Gut Directed Hypnotherapy: With a licensed practitioner, or consider the Nerva App.
- Sleep: Ensuring adequate sleep hygiene can help to regulate the nervous system and support pain tolerance.
- Vagus Nerve Support: The vagus nerve is the main nerve connecting the gut and the brain. Activities that help to improve vagal nerve tone and function include meditation, EFT tapping, breathwork and yoga.
For advanced support, if you have experienced trauma and/or ongoing psychological distress, working with a trained therapist on evidence-based therapies for trauma can help you work through past experiences in a positive way (14).

You May Want To Read: Gut-Directed Hypnotherapy: Promising Therapy for IBS
Rebalance Microbiome
Considering that dysbiosis in the gut can contribute to hypersensitivity, then supporting a healthy and diverse microbiome would be a key target area! We can support our gut microbiome by ensuring our diet has optimal amounts of fiber, prebiotics to feed good bacteria, as well as consuming adequate amounts of nutrients like zinc, Vitamin C and potassium that support gut functioning and proper motility.
Fascinatingly, eating good quality fermented foods regularly such as sourdough bread, kefir, tempeh, miso and unpasteurized sauerkraut (1 tbsp) have also been shown to improve the diversity of our gut and lower inflammation. This refers to foods that have been fermented for preservation and/or flavoring purposes, not to be confused with FODMAPs which are sugars that are easily fermented in our large intestine. For more on low FODMAP fermented foods, read our FODMAP and Food Processing series articles.
Probiotics
To date, research in animal studies have shown that probiotics including lactobacillus and bifidobacterium may help to improve visceral sensitivity and tolerance to pain by modulating the intestinal barrier, improving nerve tolerance and regulating inflammatory responses (2,10). However, exact strains and treatment protocols have not yet been confirmed as more research needs to be done in human studies.
Keep in mind that if you are considering trialing a probiotic, we recommend avoiding during the Elimination and Challenge phase of the low FODMAP diet. This is because they generally have an adjustment phase that may considerably change digestive symptoms and therefore affect your results. To be safe, always consult with a Registered Dietitian for the right type, timing and product for your needs and goals.

Want to understand more about probiotics and IBS? Check out our article, IBS & Probiotics: Should I Take Them?
It is not advised to do an elimination diet on your own, as excessive restriction of foods can lead to gut microbiome disruption and ultimately worsen symptoms, increase risk for nutrient deficiencies and perpetuate increased food anxiety long term.
Reduce Triggers Causing Pain
Elimination Diet
Food intolerances can cause bloating, gas and stool changes due to undigested food materials in your intestinal tract. This can further exacerbate pain, as well as potentially increase inflammation in your gut which may further degrade the health of your gut and exacerbate visceral hypersensitivity.
Consider working with a Registered Dietitian on an evidence-based elimination diet to help identify your personal food intolerances and sensitivities. It is not advised to do an elimination diet on your own, as excessive restriction of foods can lead to gut microbiome disruption and ultimately worsen symptoms, increase risk for nutrient deficiencies and perpetuate increased food anxiety long term.
Low FODMAP Diet
As you may know by now being a loyal reader of FODMAP Everyday® (we hope!), the low FODMAP diet is the most well studied elimination diet process to help manage the symptoms of IBS like abdominal pain, bloating and distention. The low FODMAP diet involves reducing types of carbohydrates known as FODMAPs that are poorly absorbed in the small intestine leading to rapid fermentation. This process leads to increased fluid in the gut, as well as gas production. For the person without IBS, this would not cause much change in comfort levels and trigger pain.
However, for those with IBS and visceral hypersensitivity, this fermentation can trigger intestinal nerves to send a signal to the brain and we respond by recognizing we are in pain. Thus, reducing FODMAPs in the diet for 4-6 weeks under the guidance of a Registered Dietitian, and then strategically testing them back in (the Challenge Phase) to identify personal tolerance levels can greatly help someone to manage the symptoms caused by visceral hypersensitivity to a more manageable level (17).
To Learn More About The Low FODMAP Diet Read: Low FODMAP Diet Basics
Reduce Pressure On The Abdomen
With visceral hypersensitivity, even normal levels of pressure/ stimulation can lead to increased pain. You may want to try reducing pressure on your abdomen such as wearing loose fit clothing, rather than tight waistbands and shirts that put pressure on your stomach and abdominal organs.
Consider Peppermint Capsules
Enteric coated peppermint oil capsules have been shown to effectively reduce gas, pain and abdominal discomfort associated with IBS in the most up to date meta analyses (1). Peppermint (menthol and methyl salicylate) act as a muscle relaxant and produce an antispasmodic effect in the bowels which can reduce gas, pain and cramping sensations, thereby reducing pain associated with visceral hypersensitivity.
Ginger Root
Similar to peppermint oil, ginger root has been shown to reduce intestinal muscle spasms as well as improve gut motility. This can help to relieve bloating, as well as prevent constipation which can trigger abdominal pain and heightened feelings of distention (as backed up stool puts more pressure on the intestines).
The Takeaway
Visceral hypersensitivity is a very complex symptom of IBS that involves a disruption in gut-brain communication and pain tolerance, and there is much more we need to learn and understand about its development and how to manage it. However, it is clear that supporting our gut-brain connection and supporting a healthy microbiome, as well as identifying food intolerances and reducing potential triggers, can help you to manage symptoms and not let your pain control you!
If you want to identify food intolerances through a structured elimination diet like low FODMAP, and build gut healthy habits that can help to improve visceral hypersensitivity, working with a specialized Registered Dietitian is integral to your success! Check out our Global Dietitian Directory.
References:
1. Alammar, N., Wang, L., Saberi, B., Nanavati, J., Holtmann, G., Shinohara, R. T., & Mullin, G. E. (2019). The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data. BMC complementary and alternative medicine, 19(1), 21. https://doi.org/10.1186/s12906-018-2409-0
2. Arslanova, A., Tarasova, A., Alexandrova, A., Novoselova, V., Shaidullov, I., Khusnutdinova, D., Grigoryeva, T., Yarullina, D., Yakovleva, O., & Sitdikova, G. (2021). Protective Effects of Probiotics on Cognitive and Motor Functions, Anxiety Level, Visceral Sensitivity, Oxidative Stress and Microbiota in Mice with Antibiotic-Induced Dysbiosis. Life (Basel, Switzerland), 11(8), 764. https://doi.org/10.3390/life11080764
3. Boeckxstaens G. E. (2018). The Emerging Role of Mast Cells in Irritable Bowel Syndrome. Gastroenterology & hepatology, 14(4), 250–252.
4. Campous, M. (2021). Leaky gut: What is it, and what does it mean for you?. Health. Harvard. Edu. https://www.health.harvard.edu/blog/leaky-gut-what-is-it-and-what-does-it-mean-for-you-2017092212451
5. Chiaffarino, F., Cipriani, S., Ricci, E., Mauri, P. A., Esposito, G., Barretta, M., Vercellini, P., & Parazzini, F. (2021). Endometriosis and irritable bowel syndrome: a systematic review and meta-analysis. Archives of gynecology and obstetrics, 303(1), 17–25. https://doi.org/10.1007/s00404-020-05797-8
6. Farzaei, M. H., Bahramsoltani, R., Abdollahi, M., & Rahimi, R. (2016). The Role of Visceral Hypersensitivity in Irritable Bowel Syndrome: Pharmacological Targets and Novel Treatments. Journal of neurogastroenterology and motility, 22(4), 558–574. https://doi.org/10.5056/jnm16001
7. Kendroud, S., Fitzgerald, L. A., Murray, I., & Hanna, A. (2017). Physiology, nociceptive pathways.
8. Kolacz, J., Kovacic, K. K., & Porges, S. W. (2019). Traumatic stress and the autonomic brain-gut connection in development: Polyvagal Theory as an integrative framework for psychosocial and gastrointestinal pathology. Developmental psychobiology, 61(5), 796–809. https://doi.org/10.1002/dev.21852
9.Liu, S., Hagiwara, S. I., & Bhargava, A. (2017). Early-life adversity, epigenetics, and visceral hypersensitivity. Neurogastroenterology and motility, 29(9), 10.1111/nmo.13170. https://doi.org/10.1111/nmo.13170
10. Ma, X., Mao, Y. K., Wang, B., Huizinga, J. D., Bienenstock, J., & Kunze, W. (2009). Lactobacillus reuteri ingestion prevents hyperexcitability of colonic DRG neurons induced by noxious stimuli. American journal of physiology. Gastrointestinal and liver physiology, 296(4), G868–G875. https://doi.org/10.1152/ajpgi.90511.2008
11.Ramsay, D. B., Stephen, S., Borum, M., Voltaggio, L., & Doman, D. B. (2010). Mast cells in gastrointestinal disease. Gastroenterology & hepatology, 6(12), 772–777.
12.Shrestha, B., Patel, D., Shah, H., Hanna, K. S., Kaur, H., Alazzeh, M. S., Thandavaram, A., Channar, A., Purohit, A., & Venugopal, S. (2022). The Role of Gut-Microbiota in the Pathophysiology and Therapy of Irritable Bowel Syndrome: A Systematic Review. Cureus, 14(8), e28064. https://doi.org/10.7759/cureus.28064
13. Staudacher, H.M., Black, C.J., Teasdale, S.B. et al. (2023). Irritable bowel syndrome and mental health comorbidity — approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol 20, 582–596. https://doi.org/10.1038/s41575-023-00794-z
14. Trauma-Informed Care Implementation Resource Center. (n.d). What is Trauma?. Traumainformedcare.chcs.org. https://www.traumainformedcare.chcs.org/what-is-trauma/
15.Visceral Hypersensitivity. (2022, May 11). my.cleavlandclinic.org. https://my.clevelandclinic.org/health/diseases/22997-visceral-hypersensitivity#:~:text=Visceral%20hypersensitivity%20means%20that%20your,organs%20might%20cause%20you%20discomfort.
16. Walker, M. M., Warwick, A., Ung, C., & Talley, N. J. (2011). The role of eosinophils and mast cells in intestinal functional disease. Current gastroenterology reports, 13(4), 323–330. https://doi.org/10.1007/s11894-011-0197-5
17. Webber, S. (2019). Gut Hypersensitivity and IBS. monashfodmap. https://www.monashfodmap.com/blog/gut-hypersensitivity-and-ibs/
18. Zhou, Q., Zhang, B., & Verne, G. N. (2009). Intestinal membrane permeability and hypersensitivity in the irritable bowel syndrome. Pain, 146(1-2), 41–46. https://doi.org/10.1016/j.pain.2009.06.017