Irritable bowel syndrome (IBS) symptoms can be debilitatingly painful, create severe bloating, affect our work and home life, and make us afraid to be far from a bathroom. Did you know that 10-15% of the population has IBS? You are not alone! Step 1 is to get an IBS medical diagnosis. Then turn to this article to learn about 12 common IBS triggers – and how you can calm those IBS attacks.

FODMAPs
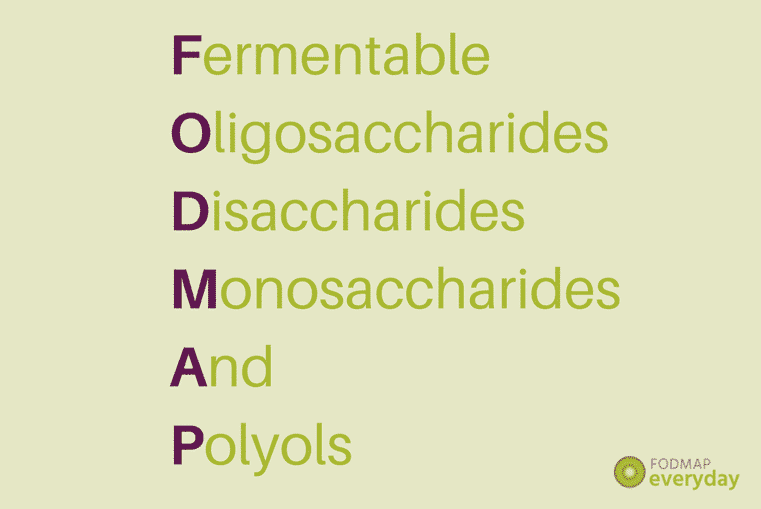
FODMAP is an acronym that stands for Fermentable, Oligosaccharides, Disaccharides, Monosaccharides and Polyols. FODMAPs are carbohydrates (sugars and fibers) that can be rapidly fermented by your gut bacteria, which can lead to pain and bloating, as well as diarrhea, and constipation.
The Low FODMAP Diet

Moving through the 3 phases of the low FODMAP diet is the best way to find out if FODMAPs are IBS symptom triggers for you, but this isn’t a try-it-on-for size diet. It is a medically directed diet, and you should only try it if your medical doctor has recommended it. If you are FODMAP sensitive, the diet is highly effective at alleviating IBS symptoms.
High FODMAP Foods

The initial Elimination Phase of the diet is the most restrictive, where you will be curtailing your ingestion of FODMAPs. Here is a very brief list of foods that are considered high FODMAP, but – and this is a huge but – many of these foods do have low FODMAP serving sizes. The low FODMAP diet is not a “no” FODMAP diet. The diet is very nuanced and complex and is meant to be undertaken with a Registered Dietitian. For instance, unripe bananas are low FODMAP, yet ripe bananas are high FODMAP.
- Apples, ripe bananas dried fruits, mangoes, pears, watermelon.
- Garlic and onions.
- Wheat, rye and barely.
- Beans and legumes.
- Cashews and pistachios.
- Avocados, cauliflower, mushrooms.
- Cow’s milk.
- Agave, honey and molasses.
Hormones

Hormones can make IBS symptoms feel worse. This can happen during puberty; days 1 and 2 of your menstrual cycle (or really at any point); women with PCOS, an endocrine disorder, have a higher incidence of IBS; birth control pills, pregnancy, HRT (hormone replacement therapy), estrogen suppression medications, and menopause can all influence IBS symptoms; and women with endometriosis are 3.5 times more likely to also have IBS symptoms.
Gluten

Gluten is the protein found in wheat, barley, and rye, and is a possible trigger for IBS symptoms. If you are celiac, then you should avoid gluten completely, but that is a separate issue from IBS. There is a condition called non-celiac gluten sensitivity (NCGS), sometimes referred to as wheat intolerance, which can produce gastrointestinal symptoms. Your gastroenterologist can screen you for celiac. If you are not celiac, but still experience digestive discomfort when eating gluten-containing foods, then it is time to discuss the issue further with your medial team.
Caffeine

Caffeine is a gut irritant and can trigger IBS symptoms; on the other hand, it can also help bring on a bowel movement which, if you are constipated, can be helpful.
Alcohol

Alcohol is also a gut irritant. When we say drink with moderation we mean from a possible impairment perspective, as well as from a digestive one! Know your tolerances.
Fatty Meals

Fatty foods can lead to digestive upset. Especially when eaten in quantity. You know the saying about potato chips; you can’t have just one (or two, or three…). So, how do you react with fat-laden meals? IBS flaring up? It could be the fat.
Spicy Foods

Chiles (or chilis or chillies, depending on where you are from) contain capsaicin, which is a known gut irritant. As with all IBS-triggering foods, reactions are highly individual. Some of you hot heads love a mouth-burning meal and suffer no repercussions. But if the tiniest sprinkle of cayenne, drizzle of hot sauce, or jalapeno garnish send you into IBS agony, you might want to hold back on the spicy additions.
Fiber

Fiber is important for our overall gut health. And here is the kicker: when it comes to IBS symptoms, sometimes they are brought on because you have too much fiber in your diet, sometimes not enough, and other times, it is because you are eating the wrong kind of fiber for you. Working with a Registered Dietitian (RD) is the best way to assess your needs.
Dehydration

There is something called the Bristol Stool chart; it shows, in graphic detail, what the 7 types of stools look like. They range from Type 1 Severe Constipation (hard little nuggets) to Type 7 Severe Diarrhea. If you look at the chart and most identify with Type 1 or Type 2, dehydration could be one of your factors. Staying hydrated can aid in alleviation of constipation – and its accompanying gut discomfort.
Eating Patterns

There are many kinds of eating patterns. Do you skip meals? Or maybe you graze all day long? Some folks have been jumping on the “intermittent fasting” bandwagon (not supported by our dietitians, BTW). Maybe you undereat, or overeat? Any and all of these eating patterns can trigger IBS symptoms. Those of us suffering with IBS do best with consistent meal patterns. Aim at consuming enough food and water at every meal for maximum nutrition and to keep your digestive track steadily humming. BTW, large meals do tend to aggravate digestion in general.
Stress & Anxiety

Despite its prevalence, the exact cause of IBS is still unknown. The most promising area of IBS research concerns the “gut-brain axis,” which is a shorthand term for the way the brain and gastrointestinal tract communicate. If you’ve ever had “butterflies in your stomach” or an urgent need for the bathroom before an exciting or upsetting event, you’ve experienced the gut-brain axis in action.
Stress can stimulate symptom flare-ups in IBS; bouts of IBS are stressful. This can become a vicious cycle. When you feel anxious, it increases your sensitivity to IBS symptoms, including pain, gas and diarrhea. Stress can make it more difficult to eat right, too, which can have secondary effects on your IBS.
Taking steps to alleviate stress can drastically improve effects of IBS. A few simple things you can do to help manage stress—and, in turn, your symptoms of IBS—include practicing mindfulness meditation and exercising. Gut-directed hypnotherapy, and self-administered programs, such as Nerva, have been clinically proven to work!
The Takeaway

IBS affects 10 to 15% of the world’s population – and is believed to be under-diagnosed. Do not self diagnose; please see your General Practitioner or Gastroenterologist for a medical diagnosis. While science does not know what causes IBS, and there is no cure for the disorder, we do know what can exacerbate IBS symptoms, and also what can be done to calm our digestive system, as outlined in this article.
The low FODMAP diet is a medically directed, clinically proven diet (not a fad) that has been shown to alleviate symptoms in up to 75% of those suffering with IBS. Knowing your hormonal status, and relationship with gluten, caffeine, alcohol, fat, spicy foods, fiber, hydration, eating patterns, and stress and anxiety can help temper your IBS flares. Working with a Registered Dietitian is the surest way to symptom-free health.







