If you experience both irritable bowel syndrome (IBS) and anxiety, you are not alone. These two conditions occur together more often than you may have realized.
A US-based study from 2023 looked at over 1 million IBS patient hospitalizations from 4000 hospitals over a 3-year period. The findings? More than 38% of those had anxiety and 27% had depression, more than double the rate of anxiety and depression found in those without IBS.

Reasons for anxiety and IBS existing together are not exactly known, but it is becoming increasingly understood that the gut-brain axis as well as increased rates of disordered eating play a role. Let’s get into these reasons for today’s article, as well as how you can help improve mood and anxiety when you have IBS!
IBS & The Low FODMAP Diet

At FODMAP Everyday we educate about a broad range of digestive issues, with a focus on the low FODMAP diet. This article addresses the intersection of IBS and anxiety, whether you are following the low FODMAP diet or not. Specifics for those with anxiety and following the diet are discussed later in the article.
What is Anxiety?

According to the American Psychological Association1, anxiety is defined as “an emotion characterized by feelings of tension, worried thoughts, and physical changes like increased blood pressure.”
The word “anxiety” is often used interchangeably with “fear”, but they are not the same. Anxiety is considered future-oriented and a long acting response to a broad or vague threat. Whereas fear is considered “appropriate” (there is an actual threat present) and is present-oriented and short lived. In simpler terms, anxiety is considered an emotion oriented around a threat or stressor that “might” happen (but not guaranteed), whereas fear is directly related to a present threat.

Psychological disorders like anxiety should be diagnosed by a psychiatrist2, a medical doctor who can diagnose and treat mental health conditions. There are various types of anxiety disorders3 including:
- Generalized anxiety disorder
- Panic disorder
- Specific phobias
- Agoraphobia
- Social anxiety disorder
- Separation anxiety disorder
- Selective mutism
Like IBS, anxiety disorders can severely impact quality of life and cause people to avoid situations that trigger their symptoms such as school, work and relationships. In general understanding for a person to be diagnosed with an anxiety disorder, the anxiety must:
- Be out of proportion to the situation
- And/or be age-inappropriate
- Hinder their ability to function normally in everyday life
Anxiety vs. Stress

Many people consider anxiety and stress to be the same, but they are different. Both are emotional responses, however stress is typically caused by an external trigger – for example: a work deadline. Anxiety is defined by persistent, excessive worries that don’t go away even in the absence of a stressor.
Both anxiety and stress have overlapping symptoms which may include:
- Insomnia
- Difficulty concentrating
- Fatigue
- Muscle tension
- Digestive symptoms
- Irritability
To read about IBS and Stress: Common Causes and Solutions
The Gut-Brain Axis
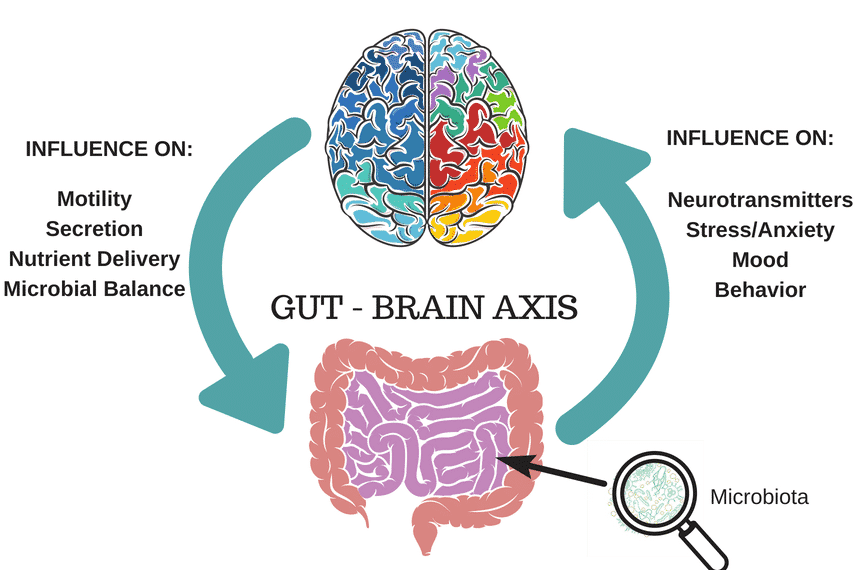
Did you know your gut and brain are connected and constantly communicating with each other through nerve endings, neurochemicals and bacteria? The gut is referred to as our “second brain”, and the connection is called the gut-brain axis.
The largest nerve in the gut-brain connection is the vagus nerve4. The vagus nerve represents the main component of the parasympathetic nervous system, which oversees a vast array of crucial bodily functions, including control of mood, immune response, digestion, and heart rate.
Our gut-brain axis is based on a very complex system, including the vagus nerve but also hormonal and immune links, and the influence of our gut microbiota in order to regulate our gastrointestinal homeostasis and connect emotional and cognitive areas of the brain with gut functions. For this reason, our mood is heavily influenced by our gut health and vice-versa.
Let’s get into how the gut-brain axis may link IBS and mood disorders like anxiety.
Anxiety & IBS

Although figures vary across the world, as mentioned above a 2023 US-based study estimated around 40% of adults with IBS also have anxiety5, double the rates of those without IBS.
While anxiety may worsen IBS symptoms, it is not thought to directly cause IBS to develop. However, more recent research6 has shown that IBS may share genetic pathways with mood and anxiety disorders.
IBS is considered a chronic, functional gut disorder and as you already know, many with the condition experience chronic pain. In general studies have shown that more than half of adults with chronic pain experience anxiety and depression.
Many with chronic pain and IBS experience limitations at work, difficulty completing daily tasks and errands, and taking part in social activities which can be linked with anxiety around symptoms7 and how their bowel habits may interfere.
Anxiety and IBS may connect in a few different ways:
Anxiety: Impact on Microbiome

The heightened inflammation8 that is triggered by stress and anxiety may trigger blooms of pathogenic bacteria that encourage dysbiosis and leaky gut syndrome. These include bacteria like Salmonella, Shigella, Campylobacter, invasive E coli, and Yersinia.
This inflammation is related to the release of catecholamines – you may know adrenaline and noradrenaline – which are released by adrenal glands when your brain senses a stressor/ threat.
With IBS, there is generally dysbiosis present, which is defined as an imbalance of healthy and pathogenic bacteria in our gut microbiome. Anxiety may potentially make this worse and/or contribute to symptoms. Ideally we want a diverse and healthy microbiome, with a higher concentration of good gut bacteria to prevent disease, regulate digestive function, and support a health gut-brain axis.
Changes in Eating Patterns

Like stress, anxiety can trigger changes in eating patterns. When you feel stress, worry or anxiety, do you eat any differently?
For many with anxiety, they experience changes in their eating behaviors. Some people tend to lose their appetite when going through a rough patch of anxiety, and decrease the amount of food they eat. This may result in eating less nutritious foods that include fiber and nutrients that support our gut heath.
For others however, both stress and anxiety may promote their intake of highly palatable foods (sugary, fatty, salty). These types of foods can also influence which types of bacteria thrive, and tend to support pathogenic bacteria.
Further, those with anxiety may increase their reliance on convenience type foods such as frozen or packaged foods due to lower motivation for self-care, especially if anxiety is also present with depression.
Vagus Nerve Dysfunction

The vagus nerve is the direct link from our brain to our gut microbiome9. This important nerve carries signals from our digestive system and organs to the brain and vice versa.
Vagus nerve function is very important for IBS and many with IBS exhibit reduced vagal nerve tone. Poor vagal function/tone can lead to:
- Altered gut motility – too slow or fast movement
- Disruptions in hunger/fullness hormones – leading to overeating, weight gain
- Inflammation gut symptoms – bloating, gas, wind, nausea
- Mood/anxiety changes
Gut Inflammation & Dysbiosis

Going back to the gut-brain connection, our gut microbiota affect processes related to our nervous system such as production of neurotransmitters, and hunger/fullness hormones). Did you know that over 90% of serotonin is produced in the gut10 (our happy hormone)?
We are learning that IBS is linked with intestinal inflammation and dysbiosis, and this weakened intestinal environment may impact the production and regulation of important hormones and neurotransmitters that regulate mood.
How to Improve Mood & Anxiety

Our brain is made of billions of nerve cells, called neurons. Communication between neurons, an electric or chemical signal between brain cells, allows the brain to work properly. We often think about nutrition and lifestyle support for our body – but what about the brain? Our brain is an important organ and requires many nutrients to function properly.
While some may absolutely benefit from medications for anxiety disorders, there is also lots you can do to support the health of your brain through dietary and lifestyle changes, especially if you also have IBS. Good nutrition also helps medications to work more effectively.
Let’s explore the key dietary and lifestyle changes to help support stable mood and anxiety.
Support the Gut Brain Axis

A diversity of plant foods in the diet has been shown to help improve gut microbiome diversity. Although we don’t know yet how to quantify a healthy gut microbiome, researchers agree that a diverse microbiome with many types of species is key to good gut health. However, many living with a digestive disorder like IBS are often hesitant to include more of them, not knowing how their gut will react. Avoiding plant based foods is not the answer, as having minimal plant diversity in your diet can actually harm your gut microbiome in the long term, which can make symptoms worse.
Listen To Our Q&A With the Author Leigh Merotto RD MHSc on The Overlap Between IBS & Anxiety
A Note on the Low FODMAP Diet

The low FODMAP Diet is a dietary approach that was developed by researchers at Monash University. It is aimed at helping individuals manage uncomfortable digestive symptoms, particularly those associated with IBS. The acronym FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are types of carbohydrates (sugars) that are poorly absorbed by the small intestine, and cause symptoms like bloating, gas, cramping and diarrhea.
This article on IBS and anxiety is intended for those with IBS, whether they are following a low FODMAP Diet or not. The food recommendations that follow do not include serving sizes. For those following the low FODMAP diet, please use your Monash University and FODMAP Friendly smartphone apps for specific serving size information. As always, speak to your Monash trained dietitian for personalized support with the low FODMAP Diet.
Diet: Plant-Based Foods, Low FODMAP, Hydration, Supplementation & Professional Guidance
- Go Low and Slow: Try adding in 2-3 new plant-based foods each week and slowly work up to a more plant-forward diet. This helps your gut microbes learn to tolerate the increase in fiber and prebiotics.
- Hydrate Well: Make sure to hydrate well when including more plant-based foods, as we need enough water to help fiber move through the gastrointestinal tract.
- Focus on low FODMAP foods: Focus on low FODMAP plant-based foods to help minimize IBS symptoms while improving your intake of fiber, polyphenols, and prebiotics.
- Consider FODZYME: For those with lactose, fructan and/or GOS intolerances, FODZYME is an enzyme blend that breaks down these FODMAPs before they get fermented by gut bacteria. This can aid in digestion of foods like garlic and onions, nuts and seeds, beans, oat milk and green peas.
- Work with a specialized gut health Dietitian: If you have anxiety about adding new foods (in order to help your anxiety), then this can become a vicious cycle. If you’ve found yourself with a very restricted diet and are hesitant to increase variety, working with a Dietitian can be incredibly instrumental in repairing your relationship with food and building a better diet to both support your digestive system and your mood/mental health.
Gut Directed Hypnotherapy

Gut directed hypnotherapy is a type of hypnosis that involves discussion and education about the digestive system, as well as induction of a hypnotic state in order to help normalize digestive functioning. A 2024 systematic review and meta analysis11 looked at several brain-gut behavioral treatments on abdominal pain in IBS and found that gut-directed hypnotherapy was helpful for patients, although not superior to the other strategies looked at.
For those who have anxiety around removing foods and/or deal with an eating disorder or disordered eating, gut directed hypnotherapy can be a helpful strategy to help manage symptoms instead of an elimination diet like the low FODMAP diet. There are registered hypnotherapists who offer this service, otherwise Nerva is a gut-directed hypnotherapy app with good clinical support behind it.
To learn more about Gut Directed Hypnotherapy: Promising Therapy for IBS
Mindful Eating: Identify Your Hunger

It can be helpful to ask yourself if you’re experiencing emotional hunger or true physical hunger12, to determine how to respond to your body’s needs.
Physical Hunger often comes on gradually and is felt in the stomach. We can usually satisfy it with a variety of tastes, flavors and textures.
On the other hand, emotional hunger which can be triggered by anxiety and stress comes on suddenly and is often felt in your head or thoughts. It may cause you to eat more than normal, and is hard to satisfy.
Notice if your hunger may be triggered by stress, emotions or anxiety. Consider a self-care strategy to help calm your emotions before reaching for food:
- Take a walk (remove yourself from the situation)
- Exercise
- Call a friend
- Gratitude journal: write down what you are thankful for, or what would make a perfect day, etc.
- Yoga: try a YouTube or online class (We have a series for you)
- Take a hot bath or shower
As we know, over-eating or reaching for options that are not ideal for our gut may trigger IBS symptoms which then can make both the anxiety and our gut symptoms worse.
Support Stable Blood Sugars & Hunger

A huge trigger for feelings of anxiety is blood sugar lows/crashes. Have you ever been “hangry”? You’re not yourself when you’re hungry. Making sure to support stable blood sugar levels can go a long way in managing anxiety.
To support stable blood sugar levels:
- Eat regularly during the day, every 3-4 hours
- Include protein with meals & snacks: Turkey, chicken, canned tuna, salmon, white fish, shrimp, lactose-free dairy (greek yogurt, cottage cheese), firm tofu, edamame
- Choose good quality carbs with fiber most often as this helps for more steady release of energy for our brain, such as: whole grains (brown rice, quinoa, amaranth), potatoes, bananas, kiwi, pitted dates, blueberries
- Limit processed & refined carbs as these are more “quick” digesting and spike our energy, but lead to a crash. This includes white flours, sugary drinks (pop, soda, juice), sweets & pastries.
Eat Enough Brain Boosting Nutrients

Magnesium
Diets low in magnesium may contribute to anxiety, restlessness, and poor sleep quality, as magnesium is important for quieting the nervous system and regulating neurotransmitters involved in relaxation. Magnesium helps with protein synthesis, muscle and nerve function, regulating blood sugars, and normalizing blood pressure, all of which can play a role in mood.
General & Low FODMAP food sources of magnesium:
- Pumpkin seeds
- Firm tofu
- Tempeh
- Lentils
- Chickpeas
- Salmon
- Halibut
- Dark chocolate
- Cocoa powder
- Spinach
B Vitamins
B vitamins are needed for the metabolism of carbohydrates, maintenance of brain cells, and production of neurotransmitters. The B complex includes B1 (thiamine), B2 (riboflavin), B3 (niacin), B6, pantothenic acid, biotin, B12, folate (or folic acid in supplement form), and choline. Fatigue, irritability, poor concentration, anxiety, and depression can all be signs of a B vitamin deficiency.
Luckily, eating a diet with a mix of lean proteins, plant-based foods like whole grains, nuts and seeds, and vegetables can help ensure you get all the B-vitamins you need and not require a supplement. A varied diet is key, which we know can be difficult when you have IBS, however it will be essential to help support a healthy mood!
General & Low FODMAP food sources of the different B vitamins include:
- B1 (Thiamine): Eggs, potatoes, spinach
- B2 (Riboflavin): Eggs, lactose-free dairy products like yogurt and milk, rolled oats
- B3 (Niacin) and B6: Chicken, turkey, tuna, whole grains, bananas
- Biotin: Eggs, spinach, tomatoes
- B12: Eggs, lactose-free dairy products, meats, fish, fortified plant-milks (oat, almond), nutritional yeast
- Folate: Dark leafy greens (spinach, kale, swiss chard, collards), strawberries, oranges
- Choline: Eggs, chicken, quinoa
Fiber

Fiber is found in plant foods only, such as fruits, vegetables, whole grains, nuts, seeds, bran cereals, beans, and lentils. It promotes the growth of good bacteria and helps maintain a healthy gut microbiome. Fiber helps manage blood sugar, reduce cholesterol, support regularity, and assist with weight management. Most North Americans sadly are getting only HALF the recommended amounts!
Daily fiber goals (adults):
- Males: 35-38g
- Females: 23-25g
Short chain fatty acids (SCFAs) are produced when the friendly bacteria in your gut ferment fiber in your colon. SCFAs help metabolize nutrients like carbs and fat and may reduce the risk of inflammatory diseases, heart disease, obesity, and Type II diabetes. SCFAs are also important for energy, mood, and brain function.
Sources of general and low FODMAP fiber include:
To learn more about Fiber and IBS: What You Need To Know
Sleep Hygiene

Sleep is essential for managing both anxiety and stress. Repair and recovery occurs primarily during sleep, including muscle, brain, and bone tissues. Sleep allows our central nervous system to reset and recharge, helping regulate stress levels.
Conversely, both acute and chronic sleep deficiency can lead to increased hunger and stress hormones, making weight management and balanced eating more difficult. As we know, it can also worsen IBS and gut symptoms, so sleep is a key player when it comes to managing both mood and gut symptoms!
Learn more about How Does Sleep Impact IBS?
Reducing Anxiety Around Foods When You Have IBS

Unfortunately, disordered eating and eating disorders are more common in those with gastrointestinal conditions like IBS. It’s important to remember that our digestive system is influenced by much more than simply what we eat. How we eat (i.e., mindful eating, meal spacing), as well as stress management, sleep hygiene, hydration, bowel routines, pelvic floor health, and movement also influence our gut function and microbiome.
Some ways to support a positive relationship with food when you have IBS include:
- Do a social media detox: Influencers, celebrities, and TikTok stars share a lot of inaccurate and scary information about gut health and nutrition online. We recommend choosing to unfollow accounts that may negatively impact your mental health. Look out for red flags like promoting all-or-nothing advice, focusing on supplements first, or promoting highly restrictive diets. Taking a set amount of time off these apps can also be very helpful.
- Don’t Restrict Randomly: Keep in mind that GI symptoms can show up to 24 hours after you consume a certain food that you may be intolerant to, so just removing a food that you had right before a flare-up may be unnecessary. Using the low FODMAP diet is an evidence based way to assess food intolerances, but we want to make sure that this is well planned out and your diet is varied from a nutritional standpoint.
- Work with a Therapist: If you have suspected disordered eating and/or an eating disorder that is difficult to manage and is impacting your day to day life, working with a trained therapist can help repair your relationship with food, your body and IBS.
- Work With a Dietitian: Rather than guessing and trying to eliminate foods from your diet randomly, work with a specialized Dietitian so that you can strategically identify triggers and tolerance levels while supporting a balanced diet and a healthy relationship with food.
Learn more about The Intersection of Gut Issues and Eating Disorders
The Takeaway

IBS and anxiety often occur together and can deeply impact one’s quality of life and interaction in society such as work, social events and daily tasks. While there is more to learn about the overlap of these two conditions, understanding the gut-brain axis, and how both diet and lifestyle choices impact this connection, can help manage both of their symptoms and impacts. This includes focusing on a nutrient-dense varied diet (low FODMAP or otherwise) including adequate amounts of nutrients for brain health and the microbiome, supporting stable blood sugar levels, as well as maintaining proper sleep hygiene.
In addition, seeking professional psychological and nutrition support when needed can be incredibly impactful. Managing IBS and anxiety is not simply about eliminating symptoms but fostering a holistic approach to mental and physical health!
Any questions about IBS and anxiety? Share with us below.
Sources:
- American Psychological Association. (n.d.). Anxiety. https://www.apa.org/topics/anxiety ↩︎
- Cleveland Clinic. (n.d.). Psychiatrist. https://my.clevelandclinic.org/health/articles/22702-psychiatrist ↩︎
- American Psychological Association. (2024). More than half of adults with chronic pain experience anxiety and depression. https://www.apa.org/monitor/2024/03/chronic-pain-depression-anxiety ↩︎
- Frontiers in Psychiatry. (2018). The gut-brain axis: An important route for bidirectional communication between the gut and the brain. https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00044/full#B1 ↩︎
- SpringerLink. (2023). Prevalence of anxiety and depression in IBS patients. https://link.springer.com/article/10.1007/s11845-022-03258-6 ↩︎
- Nature Genetics. (2021). Genetic overlap between IBS and mood disorders. https://www.nature.com/articles/s41588-021-00950-8 ↩︎
- American Psychological Association. (2024). More than half of adults with chronic pain experience anxiety and depression. https://www.apa.org/monitor/2024/03/chronic-pain-depression-anxiety
↩︎ - PubMed (2019). Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213601/#R10 ↩︎
- National Center for Biotechnology Information. (2018). Vagus nerve as modulator of gut-brain axis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859128/ ↩︎
- National Center for Biotechnology Information. (2015). Gut microbiota’s role in the central nervous system and gut-brain axis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/ ↩︎
- PubMed. (2024). Systematic review and meta-analysis of brain-gut behavioral treatments for IBS. https://pubmed.ncbi.nlm.nih.gov/38777133/ ↩︎
- Young Women’s Health. (2018). Reconnecting with hunger and fullness. https://youngwomenshealth.org/wp-content/uploads/2018/09/Reconnecting-with-Hunger-and-Fullness.pdf ↩︎




