What is IBS?
An estimated 10 to 15 percent of the worldwide population suffers from irritable bowel syndrome (IBS), a chronic digestive disorder of the large intestine that causes abdominal pain, diarrhea (IBS-D), constipation (IBS-C), alternating episodes of both (IBS-M), or IBS-U (Unclassified; symptoms vary). A change in bowel habits and bowel movements are often a marker. Not every IBS sufferer will exhibit all these symptoms.
IBS is considered a “functional gastrointestinal disorder”, and now often also referred to as a gut-brain interaction disorder. It is not the same as ulcerative colitis, colon cancer, Crohn’s disease, or IBD (inflammatory bowel disease).
The symptoms of IBS are the result of abnormal intestinal motility –– too fast leads to diarrhea, too slow to constipation –– and increased sensitivity to pain. There is even something called “high stool burden”. Bloating, gassiness, bowel urgency, and mucus in the stool are also common in IBS. Weight loss or weight gain can be a side effect of IBS.
What Causes IBS?
Despite its prevalence, the exact cause of IBS is still unknown, and we don’t have diagnostic tests for it like we do for celiac disease and inflammatory bowel disease (IBD). Still, there has never been more interest in understanding and treating this complex disorder.
The most promising area of IBS research concerns the “gut-brain axis,” which is a shorthand term for the way the brain and gastrointestinal tract communicate. If you’ve ever had “butterflies in your stomach” or an urgent need for the bathroom before an exciting or upsetting event you’ve experienced the gut-brain axis in action.
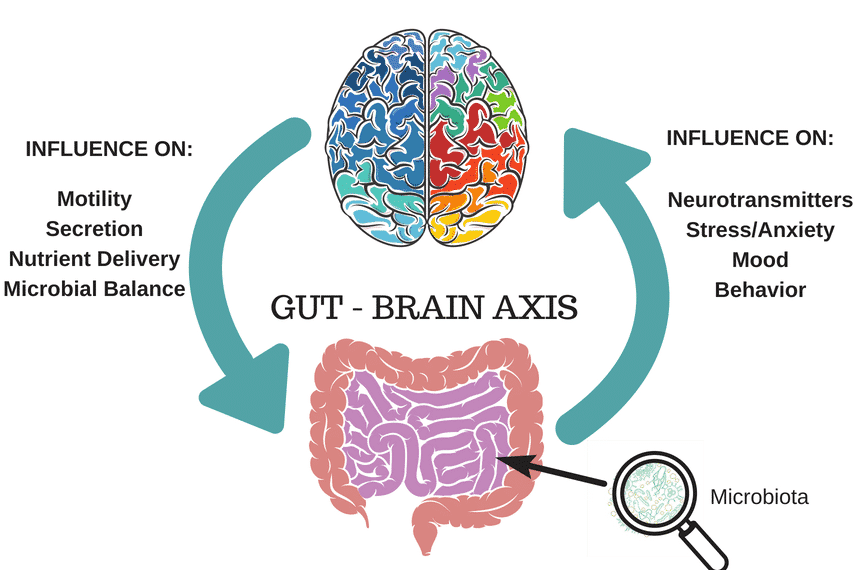
The important thing to understand is that gut-brain axis is a two-way street, with the brain influencing how the gut functions and the gut modulating how the brain functions.
Researchers suspect that disruptions in this pathway cause the intestinal motility problems and increased sensitivity that lead to classic IBS symptoms of diarrhea, constipation, and pain. Furthermore, they suggest that gut bacteria –– the gut microbiome –– play a big part in causing brain and gastrointestinal tract to miscommunicate in the first place.
How Is IBS Diagnosed?
There is no formal test for IBS that is widely used or particularly reliable*; IBS is typically diagnosed based on symptoms, after certain tests may be done which screen for diseases and conditions that present same or similar symptoms. It is very important that you do not self-diagnose. Please read our article, IBS: Step-by-Step Guide from Diagnosis to Symptom Free Living, for more information.
*(Though there is no universally applicable diagnostic tool for all IBS forms, there is a relatively new, commercially-available antibody blood test called IBS-Smart. This test measures biomarkers associated with IBS-D and IBS-M, which may be elevated following infectious gastroenteritis and presents a potential diagnostic option for post-infectious IBS-D and IBS-M. As always, consult with your trusted health professional to learn more if they believe this may be a useful tool in your diagnosis Please read our previously published article that discusses this test for more information, and discuss the advantages and limitations with your medical team.)
Gastroenterologists Can Diagnose
A gastroenterologist (GI) or MD should first review your full medical history and perform a physical exam, then will most likely order blood, urine and/or stool tests and screen you for celiac disease. Depending on your symptoms, they might also screen you for IBD (inflammatory bowel disease), Crohn’s, diverticulitis and/or endometriosis.
A colonoscopy might be recommended, and some doctors will order X-rays or CT scans, lactose-intolerance tests and/or breath tests for SIBO.
Gastroenterologist should also use the Rome IV Criteria (the Rome Foundation creates guidelines for diagnosing IBS). GIs are more likely to be familiar with this criteria than your General Practitioner.
A formal IBS diagnosis will be given when other medical issues are ruled out and your symptoms match those that are indicative of IBS, such as those presented in the Rome IV criteria.
A formal IBS diagnosis will be given when other medical issues are ruled out and your symptoms match those that are indicative of IBS, such as those presented in the Rome IV criteria.
Gut Microbial Composition
Recent scientific studies have shown that certain types of microbes are found in the gut of those who are more likely to have IBS; for instance, gammaproteobacteria seem to be in greater abundance in both children and adults who have IBS. Other pathogens, such as Clostridioides difficile, may also be contributing to IBS symptoms. Researchers are hopeful that these findings will aid in diagnostic and therapeutic approaches. In the future it might be possible to make very specific recommendations for individuals, for probiotics and prebiotics for instance, based on their unique gut microbe presentation.
The low FODMAP diet is one such approach that can alter microbial composition in a positive way for some of us with IBS.
What Makes IBS Symptoms Worse?
While there is no one thing – food or otherwise – that creates IBS, there are many things that can trigger or exacerbate symptoms. These include, but are not limited to: high FODMAP foods, dairy products, lactose intolerance, depression, stress, anxiety, spicy food, caffeine, prescription and over the counter medicines, supplements, digestive tract infections, to name a few.
How Is IBS Treated?
It’s very frustrating to hear that the cause, much less the cure, for such a common condition is still unknown, but we do have more ways of treating IBS than ever before. These interventions generally fall into three categories: dietary, pharmaceutical, and psychological.
- Dietary: The premier dietary approach for IBS –– the low FODMAP diet –– has been shown to provide significant symptom relief in 75 percent of people who try it. That’s a remarkable statistic. It’s also why our goal at FODMAP Everyday® is to help you understand and incorporate the low FODMAP diet into your everyday life. You can read more about the diet here, and then start putting it into practice with our delicious low FODMAP diet recipes.
- Pharmaceutical: Medications for IBS are *numerous but they often target only one of the predominant symptoms which is problematic if you suffer from two or more. Another drawback to using drugs for IBS is the potential for side effects.
- Psychological: The most well researched psychological interventions for IBS are cognitive behavioral therapy (CBT) and gut-directed hypnosis. These are particularly helpful for people whose symptoms are exacerbated by stress. Both CBT and gut-directed hypnosis have success rates that surpass many medications but they also require a greater time and emotional commitment.
*Alternately https://emedicine.medscape.com/article/180389-medication
To read how others handle their IBS flares, check out our article, How To Relieve An IBS Attack.
The Takeaway
It is possible to live a pain-free and symptom-free life with IBS by using the management techniques that work for you. In other words, the long term outlook is good!
Step #1 is getting an accurate diagnosis from a medical doctor or gastroenterologist, and then working with a Registered Dietitian. Your GI might suggest the low FODMAP diet, in which case FODMAP Everyday® will be of immense help. The low FODMAP diet has been clinically proven to provide relief for about 75% of the 1 in 7 people worldwide who are diagnosed with IBS. Although a doctor might not mention this, the diet is meant to be undertaken along with a RD.
Here at FODMAP Everyday® we have 1000+ recipes and hundreds of evidence-based articles written by Monash University trained dietitians (Monash researchers developed the diet). Dédé Wilson, our lead recipe developer, is Monash University trained as well, and also FODMAP Friendly Accreditedas a FODMAP educator – as is FODMAP Everyday®. So whether you need information on IBS, the low FODMAP diet, gut-friendly recipes or a community of others experiencing GI distress, you have landed at the right place.