Irritable Bowel Syndrome (IBS) is not experienced the same way by any two people. It is not a one-size fits all disorder, and treatment is not a singular approach, either. There are four IBS subtypes – IBS-D (diarrhea), IBS-C (constipation), IBS-M (Mixed; alternating loose stools and constipation), and IBS-U (Unclassified; symptoms vary). This article explores what determines your subtype, and the tailored treatment approaches.
IBS, The Low FODMAP Diet & Honing In On Proper Treatment
When I started to experience IBS symptoms, I was a fresh graduate from the University of British Columbia (Canada) bestowed with a shiny designation of “Registered Dietitian”, yet I had NO IDEA WHAT WAS GOING ON WITH MY GUT.
It was the worst. I was already dreading the diarrhea and “gut rot” that was to come at every holiday, gathering, dinner out, or even on any given day.
At one point, I drew up the most massive spreadsheet on my computer, and each day went through it with a fine-toothed comb. Was it gluten? Dairy? Sulphites? Wheat? Alcohol, etc.? But alas, no obvious pattern emerged.
Elimination Phase: 1 of 3 Phases
I eventually went on a full Elimination version of the science-based diet for IBS (Low FODMAP) that – and here comes the second dose of irony – I was already just starting to occasionally teach folks about as an RD in another RD’s practice.
I honestly didn’t think dietitians or people who ate and lived “well” in general could get such severe IBS, so it wasn’t even on my radar. Call me naïve.
Anyhow, the low FODMAP diet worked well to control about 60-75% of my symptoms: I was through the worst of it.
Sidenote: Even though I was a Dietitian myself, I should have sought out a Monash University trained, Low FODMAP & IBS Registered Dietitian (later I received this designation) when I first connected the proverbial dots as to what was going on with my digestion. It would have made the process a whole lot smoother, and most importantly, I might not have eaten so restrictively, for so long.
But I was far too proud, and unfortunately I did not, because…
Even when I felt I was eating 100% low FODMAP, and in theory should have my IBS “managed”, I still had far too many unexplained “flare-up days”, in my opinion.
Most Need Help With The Low FODMAP Diet – Even Dietitians!
Even as a dietitian, knowing the low FODMAP diet basics, and using it on myself, I struggled with some level of symptoms – namely diarrhea – because I didn’t yet know about the additional tools and strategies that were specifically for my subtype: IBS-D. That “D” folks, is for “diarrhea”.
For example, a large, low FODMAP green salad often felt like it “went right through me”, despite being “LoFo”. Later on I discovered (through research and my own lived experience) that IBS-D’ers need to pay attention to concepts like “roughage” (insoluble fibre from plant cell walls, skins, and seeds, like in salads or vegetable side dishes), sugar alcohols, large amounts of fruit/smoothies, as well as the idea of low FODMAP soluble fibre therapy (just to name a few of my eureka moments).
The diarrhea drama became further behind me as I dialed in the above concepts, and more, specific to IBS, and my subtype.
More on the sub-types, and select strategies beyond FODMAPs that can be folded into one’s treatment, below.
IBS management may go beyond the low FODMAP diet (and the other general IBS pointers listed below), and these tools and strategies often can be very SUBTYPE-DEPENDANT.
I cannot stress enough, that including a Monash University trained IBS Dietitian as part of your health care team, and in particular one that can factor in your IBS subtype in creating your individualized treatment plan, is the key to success. To find a Monash trained Dietitian, head to their FODMAP Dietitians Directory here.
I cannot stress enough, that including a Monash trained IBS Dietitian as part of your health care team, and in particular one that can factor in your IBS subtype in creating your individualized treatment plan, is the key to success.
Aside from some version of a low FODMAP Diet, my IBS-D treatment plan looks quite different from a plan I would give someone with IBS-C, and so on.

First: IBS Defined
In the past, Irritable Bowel Syndrome (IBS) was described as a type of “functional gastrointestinal disorder”- a set of symptoms that didn’t seem to have an organic cause or reliable testing to clearly diagnose.
However, IBS is now recognized as one of more than 27 disorders of gut-brain interaction (DGBI) and is a relapsing, chronic, condition that affects an estimated 7 to 15% of the global population.
IBS, like many disorders of gut-brain interaction (DGBI) diagnoses, can come with:
- Motility disturbances (the speed at which food moves through the gut is too slow, or too fast which can lead to constipation, diarrhea or both).
- Altered gut microbiota (changes in the type and number of our “gut bugs”).
- Visceral hypersensitivity (how sensitive our gut lining is to stretch and/or pressure of its contents).
- Altered central nervous system function (inappropriate responses back and forth from the gut to the brain for example).
- And more changes that play a role in each person’s individual constellation of symptoms.
Tests For IBS Diagnosis
Before IBS is diagnosed, are there any tests that should be done? Yes indeed. It is recommended by The American College of Gastroenterology (ACG) that Celiac Disease and Inflammatory Bowel Disease (IBD) are ruled out first, as these may have overlapping symptoms of IBS, yet carry serious health consequences if left undiagnosed. Additional tests might be ordered based on a person’s age, medical and family history, and specific signs and symptoms.
Should every test be ordered before arriving at an IBS diagnosis? Not necessarily. The ACG further suggests a positive diagnostic framework (as opposed to the previous mindset of a diagnostic strategy of exclusion) for patients with IBS-like symptoms in order to expedite appropriate therapy.
Do Not Self Diagnose
We also want to point out that IBS should not be self-diagnosed. Depending on where you live in the world, it might be diagnosed by a General Practitioner or a Gastroenterologist.
We also want to point out that IBS should not be self-diagnosed. Depending on where you live in the world, it might be diagnosed by a General Practitioner or a Gastroenterologist.
Once you have an accurate diagnosis, you can skip to the section of this article that is focused on your IBS subtype.
How The Rome Foundation Relates To Diagnosis
In short: Diagnosing IBS is morphing from “all the tests are coming back negative, so it’s ‘possible that it might be’ IBS”, to a clear, positive and confident IBS diagnosis based on the below “criteria”, in the absence of alarm features.
These are set forth by the Rome Foundation, which is an independent not-for-profit organization dedicated to supporting the creation of scientific data and educational information to assist in diagnosing and treating Disorders of Gut-Brain Interaction (DGBIs), formerly called Functional Gastrointestinal Disorders (FGIDs).
The Rome IV Diagnostic Criteria for Irritable Bowel Syndrome
Here is the Rome Foundation’s definition of IBS:
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following *criteria:
- Related to defecation
- Associated with a change in frequency of stool
- Associated with a change in form (appearance) of stool
* Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.
In normal terms?
Basically, IBS Is described by a combination of recurrent abdominal pain, typically 2-8 hours after eating, and changes in bowel habits (constipation, diarrhea or back and forth between the two).
Bloating, Gas & Other Symptoms
What about bloating you ask?
At this time, bloating is not a required symptom to diagnose IBS, however its presence is very frequently reported amongst those living with an IBS diagnosis, is worse in the evening, and improves overnight.
Other common symptoms of IBS may include excessive passage of gas (lots of farting/wind), abdominal distention (a visible increase in the girth of a person’s midsection), incomplete evacuation (feels like more poop needs to come out), and nausea.
Red Flags: Symptoms That Could Mean Additional Medical Issues

It’s important to note that there are some symptoms that are considered “red flags” or “alarm features” that might point to other conditions besides IBS, and that may require further medical input and testing by your health care team, such as:
- Unexplained weight loss
- Family history of bowel disease
- Rectal bleeding
- Anemia
- Fever
- Progressive or severe symptoms
- Vomiting
- Persistent daily watery diarrhea
- Age of onset of symptoms over 50 years
- Nocturnal bowel movements (needing to wake up in the middle of the night to open your bowels)
General Treatment Suggestions For All IBS Subtypes
It’s true that there are some treatments that may potentially be beneficial for all IBS subtypes across the board, including, but not limited to:
- Temporarily reducing certain high FODMAP foods (guided by a Registered Dietitian)
- Gut-directed hypnotherapy, such as Nerva
- Cognitive behavioural therapy
- Mindfulness strategies
- Herbal supplements such as Iberogast or enteric coated peppermint oil, for example
- Eating slower and chewing thoroughly
- Gentle movement
- Healthy eating modifications
- Diaphragmatic breathing
- And let’s not forget sleep
However, there are several helpful, subtype specific, tools and strategies available that you can work with your health care team to trial as a part of the plan to treat your specific constellation of IBS symptoms.
The Four IBS Subtypes

Irritable Bowel Syndrome (IBS) is currently categorized into 4 subtypes:
- IBS-D (Diarrhea)
- IBS-C (Constipation)
- IBS-M (Mixed; alternating loose stools and constipation)
- IBS-U) (Unclassified; symptoms vary)
It’s true.
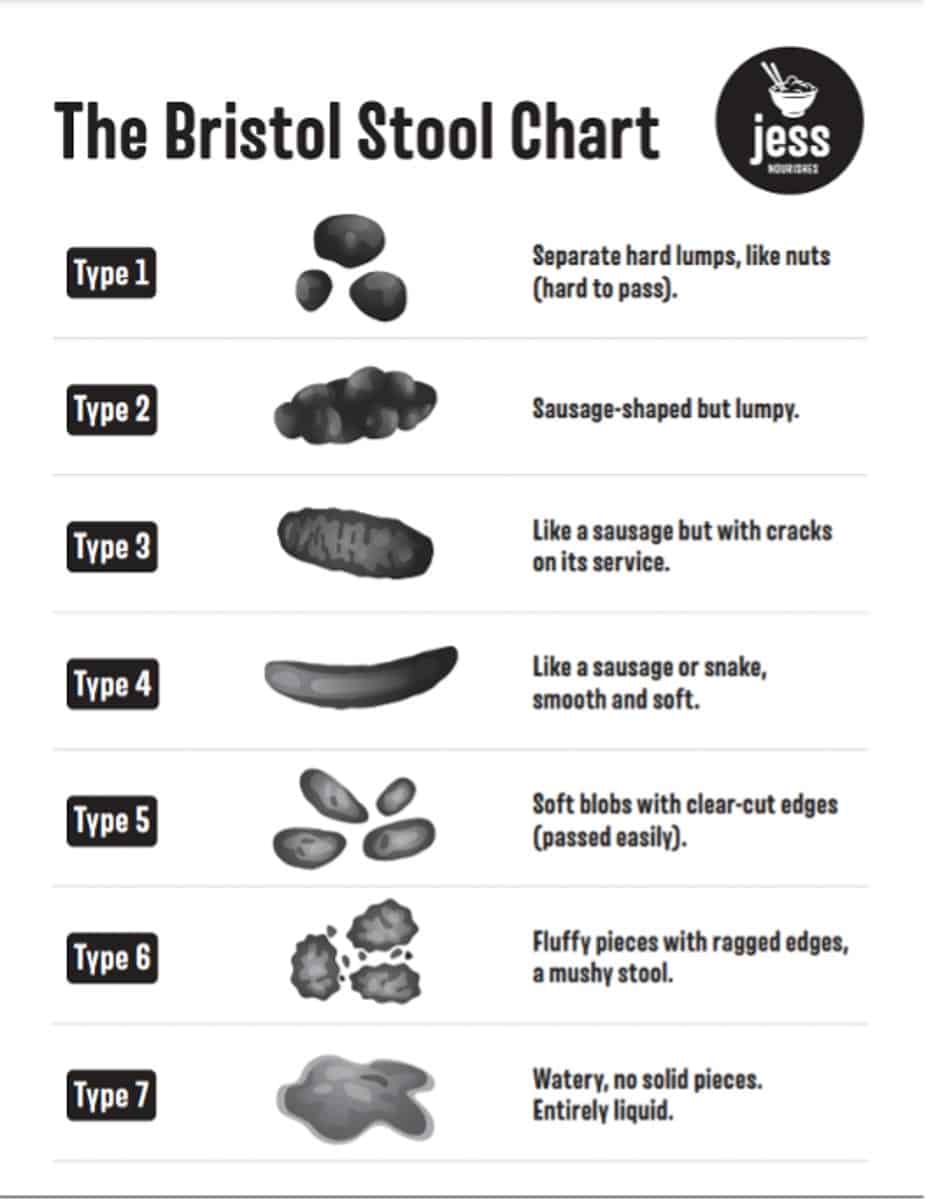
Currently IBS subtypes are based on one’s bowel habits when they are abnormal, and are evaluated using the Bristol Stool Chart and the “25% rule”, ideally using two weeks’ worth of “poop diary data”.
In other words, the form (size, shape and texture) of bowel movements your body makes are compared to the chart, which rates them from 1-7 (ranging from a 1, hard “rabbit pellet-like” poops that are difficult to pass, all the way to 7, which is essentially liquid stool with no solid pieces).
If your body tends to make the constipated types of stool (Types 1 and 2) and/or the diarrhea stools (Type 6 and 7) more than 25% of the time that you have an abnormal poop, you may fall under one of the four subtypes of IBS.
Assigning An IBS Subtype Improves Care
Although IBS folks may each have their own unique constellation of symptoms, most patients with IBS can be matched to therapies targeted to treat their particular subtype, and this can be very helpful.
On the flip side, it makes sense that mismatching treatments to the wrong subtype can potentially worsen symptoms.
I’ll give you an example:
Commonly prescribed antidepressant medications might be tricyclic antidepressants (TCAs), or selective serotonin reuptake inhibitors (SSRIs). TCAs carry a common side effect of constipation. On the flip side, one common side effect of SSRIs is diarrhea.
In addition, the same medications may be prescribed, in lower doses, to target pain for some folks with IBS.
Practitioner note: To reduce the potential stigma of using these types of medications for IBS, you can help patients think of this as not so much treating depression in someone, rather, think of it as just their digestive system may be depressed, and thus it may benefit from relatively small doses of potentially one of the aforementioned medications.
However, as you can imagine, if someone’s bowel habits are already constipated (like in IBS-C), or diarrhea (like in IBS-D) it makes sense that careful planning with one’s health care team (including factoring in their IBS subtype) would make selecting the right medication for the right person crucial in order to not exacerbate their constipation or diarrhea, respectively.

Other examples I see is someone with IBS-D, with trouble sleeping, being suggested to take a natural health product (NHP) that might make diarrhea worse (I’m looking at you high doses of magnesium); whereas someone with IBS-C and sleep issues may potentially benefit from the laxative effect of certain magnesium dosages.
A consensus recommendation by the American College of Gastroenterology echoes this sentiment: accurately categorizing folks with IBS based on their primary bowel habit is generally recognized to help improve patient therapy – and may help steer patients away from recommendations that may actually worsen symptoms.
Accurately categorizing folks with IBS based on their primary bowel habit is generally recognized to help improve patient therapy – and may help steer patients away from recommendations that may actually worsen symptoms.
Let’s look at the four IBS subtypes now, along with some quick tips and tools that I’ve gathered together for each subtype.
IBS-D: IBS with Predominant Diarrhea

Hello, it’s nice to meet you (this is my subtype)!
IBS-D is defined as more than 25% of abnormal bowel movements are loose or watery (Type 6 or 7), and less than 25% of abnormal bowel movements are hard or lumpy (Type 1 or 2). Or, IBS-D may be assigned when a person reports that most of their bowel movements are diarrhea.
People with IBS often experience an individual constellation of symptoms unique to them. In my practice, I often find urgent/loose/frequent bowel movements, bloating, gas, abdominal pain and having trouble tolerating foods high in “roughage” or beverages like coffee and alcohol are the primary struggles of IBS-D folks, and thus my recommendations target evidence-based ways to help reduce such symptoms, including:
Potential Diet to Explore:
- Low FODMAP diet
- See the 1-day Low FODMAP, low roughage, Meal Plan for IBS-D example found in my IBS-D Mini Guide on my website.
Potential Medications to Ask Your Doctor About:
- Rifaximin
- Loperamide
- Tricyclic antidepressants
Supplement Picks:
For abdominal pain:
For improved stool form:
Low FODMAP soluble fibre therapy:
- PHGG
- Acacia Senegal (I like Heather’s Tummy Fibre Brand, which I stir into moist foods or take dissolved in water)
For post-infectious IBS:
For increased food freedom, once you have completed your Challenge Phase.
FODMAP digesting enzymes like FODZYME
Things That Might Make Diarrhea Worse:
- Coffee & alcohol
- Sugar alcohols
- Large servings of “roughage” fibre like large salads
- High fat meals
- Eating fast/insufficient chewing
- Inulin/chicory root/ other high FODMAP foods (these can be hidden within “flavorings” in the U.S.)
Food Examples That May Work Well for Those with IBS-D:
- Oranges
- Rolled oats (up to ½ cup)
- Peeled cucumber
- Sourdough
- Cooked & cooled rice or potato
- Other low FODMAP foods & resistant starch sources
Note: Those with diarrhea symptoms can also closely resemble other diagnoses (or have additional issues) such as bile acid malabsorption (BAM), small intestinal bacterial overgrowth (SIBO), intolerances to certain sugars, celiac disease, histamine intolerance, and pancreatic insufficiency.
Always work with your health care team (including a Registered Dietitian) to determine the proper testing, treatment and diet to follow, as some issues are more serious than others if left untreated (such as celiac disease).
What About SIBO, ISO And IBS-D?
Captivatingly, a large portion (an estimated 50-80%) of my fellow IBS-D friends have Small Intestinal Bacterial Overgrowth (SIBO). There is also a fairly new “kid on the block”: Intestinal Sulphide Overproduction (ISO).
The gut bacteria running rampant in SIBO have recently been uncovered to be actually very few, specific kinds.
For SIBO, research associates mainly two species of E. coli, E. coli K-12, and E. coli BL21(DE3) and two Klebsiella species (K. aerogenes and K. pneumoniae) as the gut bugs dominating someone with SIBO’s microbiome.
For ISO, research tags Fusobacterium and Desulfovibrio as “it” when it comes to linking increased breath H2S (hydrogen sulphide) levels to increased diarrhea in those with IBS-D.
Hydrogen gas detected on a breath test that rise more than 20ppm above baseline is considered a “positive” and may point in the direction of SIBO.
Recently, there has been a breath test invented that can detect all three gasses (methane, hydrogen, and hydrogen sulphide), whereas prior there was only the ability to measure methane and hydrogen breath gasses.
Currently, there is no consensus on the rise of hydrogen sulphide gas (H2S) of a breath test needed for a “positive” result; but at the time of writing, certain studies suggest 3 ppm, while others suggest 5 ppm as the benchmark for ISO.
Treatment for SIBO suggested in research studies is typically antibiotic therapy (such as Rifaximin for 2 weeks), and this may also be the suggestion for ISO (with the potential for the addition of Bismuth. Yes, that’s good ol’ Pepto).
If you have IBS-D, it could be worthwhile to discuss SIBO and/or ISO and their treatment options with your Doctor.
I could talk all day about diarrhea (in fact, I do), but perhaps you might wish to follow me on Instagram or visit jessnourishes.com for more diarrhea fun, or grab my IBS-D Mini-Guide here.
IBS-C: IBS with Predominant Constipation
IBS-C is defined as less than 25% of abnormal bowel movements are loose or watery (Type 6 or 7), and more than 25% of abnormal bowel movements are hard or lumpy (Type 1 or 2). Or, IBS-C may be assigned when a person reports that most of their bowel movements are constipation.
People with IBS often experience an individual constellation of symptoms unique to them. In my practice, I often find hard/dry/infrequent bowel movements, bloating, gas, nausea, abdominal pain and getting in enough (less bloating) fibre sources are the primary struggles of IBS-C folks, and thus my recommendations target evidence-based ways to help reduce such symptoms, including:

Potential Diet to Explore:
- Low FODMAP diet
- See the 1-day Low FODMAP Meal Plan for IBS-C example found in my IBS-C Mini Guide on my website. This meal plan is high in roughage. See notes below.
Potential Medications to Ask Your Doctor About:
- Chloride channel activators (ex. Lubiprostone)
- Guanylate cyclase activators (ex. Linaclotide)
- SSRI antidepressants
- PEG products
Supplement Picks:
For abdominal pain:
Enteric coated Peppermint oil. Note that many folks with IBS-C may experience reflux as a part of their constellation of symptoms, and some peppermint products may aggravate reflux for some.
For nausea:
Ginger
For bloating and increased food freedom, once you have completed your Challenge Phase.
FODMAP digesting enzymes like FODZYME
My (low FODMAP) Fibre Pick for You*:
Insoluble fibre, for example: KFibre brand
Things That May Help Speed Up the IBS-C Gut or Soften Stools:
- Coffee
- Magnesium citrate
- Water
- Physical activity/movement
- Abdominal massage (clockwise in direction, following the path to “out” of the large intestine)
Food Examples That May Work Well for Those with IBS-C:
Low FODMAP fruits or vegetables with skins (roughage)*:
- Flaxseeds
- Pecans, Walnuts, Peanuts
- Chia water
- Kiwi
- Blueberries
- Low FODMAP smoothies & salads*
*Note: Some folks with IBS-C thrive with a diet high in Low FODMAP sources of roughage, while others may not, for various reasons. See below. If you have not had a bowel movement in 5 to 7 days, do not take a fibre supplement; consult with your doctor as there may be risks, such as obstruction.
Those with IBS-C may also try a soluble fibre supplement; however, it is important to understand that some folks may have underlying issues with constipation due to factors such as lack of fibre/water, or Pelvic Floor Dysfunction (PFD).
In PFD for example, fibre supplements have the potential to worsen symptoms, or even create situations such as bowel obstruction. Always speak to your health care team about this possibility. If you are often constipated, you may be referred to a pelvic floor physiotherapist to assess the health of your pelvic floor.
What About IMO And IBS-C?
Interestingly, about 50% of those with IBS-C may also have an overgrowth of a certain kind of gut microbe (not a bacterium, but rather “archaea”) in their intestines (like Methanobrevibacter smithii, if you want to geek out) which loves to create constipating methane gas.
In other words, Intestinal Methanogen Overgrowth (IMO) is often an additional layer to those with IBS-C.
Methane levels detected on a breath test that rise more than 10 ppm is considered a “positive” and may point in the direction of IMO.
Currently, the treatment for IMO suggested in research studies is “dual antibiotic therapy”, which typically is Rifaximin combined with another antibiotic.
If you have IBS-C, and are experiencing stubborn gas and bloating (some of the most commonly reported symptoms of those with IMO), it could be worthwhile to discuss IMO with your Doctor so that they may guide you with regards to your IBS-C, IMO, breath testing, treatment, and more.
For a little more, you may wish to grab my IBS-C Mini-Guide here.
IBS-M: IBS with Mixed Bowel Habits
IBS-M is defined as more than 25% of abnormal bowel movements are loose or watery (Type 6 or 7), and more than 25% of abnormal bowel movements are hard or lumpy (Type 1 or 2). Or, IBS-M may be assigned when a person reports that their bowel movements go back and forth between constipation and diarrhea.

People with IBS often experience an individual constellation of symptoms unique to them. In my practice, I often find cycling between hard and loose bowel movements, bloating, gas, abdominal pain and getting enough (less bloating) fibre sources are the primary struggles of IBS-M folks, and thus my recommendations target potential tools to help reduce their metaphorical roller coaster of a bowel movement pattern (constipation to diarrhea, and repeat!) and other symptoms. The IBS-M specific tools and strategies I use in my practice may include:
Potential Diet to Explore:
- Low FODMAP diet
- See the 1-day Low FODMAP Meal Plan for IBS-M example found in my IBS-M Mini Guide on my website.
Potential Medications to Ask Your Doctor About:
As of 2020, there are no approved medications specifically for the treatment of IBS-M or IBS-U listed by the ACG; however, Monash University & ACG list TCA antidepressants as potentially beneficial for “global” IBS symptoms.
Supplement Picks:
For abdominal pain:
For improved stool form:
Low FODMAP soluble fibre therapy:
- PHGG
- Acacia Senegal (I like Heather’s Tummy Fibre Brand, which I stir into moist foods or take dissolved in water)
For bloating and/or increased food freedom once you have completed your Challenge Phase.
FODMAP digesting enzymes like FODZYME
Help for Constipation Days:
Consider increasing:
- Coffee
- Water
- Kiwi fruit
- Movement/exercise
Help for Diarrhea Days:
Consider decreasing:
- Coffee
- Fruits and vegetables (roughage)
Consider increasing:
- Soluble fibre
Food Examples That May Work Well for Those with IBS-M*:
- Sourdough bread
- Kiwi fruit
- Rolled oats (up to ½ cup)
- Chia puddings
- Oranges
- Popcorn
- Other Low FODMAP foods
*Note: If you have not had a bowel movement in 5 to 7 days, do not take a fibre supplement and consult with your doctor as there may be risks, such as obstruction. Those with IBS-M may have more of an underlying issue with constipation due to factors such as lack of fibre, IBS-C, or Pelvic Floor Dysfunction (PFD).
Fibre supplements or very high fibre foods have the potential to worsen the digestive picture of people with various types of constipation. Always speak to your health care team about this possibility. You may be referred to a pelvic floor physiotherapist to assess the health of your pelvic floor, or to an IBS-trained Registered Dietitian to help with more individualized dietary advice.
What About SIBO, IMO and IBS-M?
There may also be a degree of gut dysbiosis such as SIBO or IMO involved in this subtype too. Please refer to the sections above that discuss SIBO and IMO in more detail.
Studies suggest instances of intestinal methane overgrowth (IMO) to be 24% in IBS-M, and instances of SIBO are approximately the same at 25%.
Again, these brands of dysbiosis should be discussed with your health care provider, as they are common in the context of IBS, and may require additional testing and treatment.
If you’d like my mini-guide for your IBS-M, feel free to grab it here.
IBS-U: Unclassified
Unclassified folks are assigned IBS-U when they meet the Rome IV criteria for IBS in terms of recurrent abdominal pain, yet their bowel habits cannot fit into any of the above three neat little subtype categories. In other words, someone may not experience significantly abnormal bowel patterns (more than 25% of the time having constipation, diarrhea, or both) unlike the IBS-Ds, Ms and Cs.
People with IBS often experience an individual constellation of symptoms unique to them. In my practice, I often find bloating, gas and abdominal discomfort are the primary struggles of IBS-U folks, and thus my recommendations target evidence-based ways to help reduce such symptoms, including:
Potential Diet to Explore:
- Low FODMAP diet
- See the 1-day Low FODMAP Meal Plan for IBS-U example found in my IBS-U Mini Guide on my website. You may wish to swap in a salad recipe for lunch or dinner, depending on how your body handles “roughage”.
Potential Medications to Ask Your Doctor About:
As of 2020, there are no approved medications specifically for the treatment of IBS-M or IBS-U listed by the ACG; however, Monash University & ACG list TCA antidepressants as potentially beneficial for “global” IBS symptoms.
Supplement Picks:
For abdominal pain:
For nausea:
Ginger
For bloating:
- Simethicone
- FODMAP digesting enzymes once you have completed your Challenge Phase, such as FODZYME.
For increased food freedom, once you have completed your Challenge Phase.
Try a FODMAP digesting enzymes like FODZYME,
Food Examples That May Not Work Well with IBS-U:
- Coffee
- Alcohol
- High FODMAP Foods such as:
Food Examples That May Work Well IBS-U*:
- Sourdough bread in place of whole wheat
- Rolled oats (up to ½ cup) instead of large oat servings
- Oranges
- Carrots
- Cucumbers
- Other low FODMAP foods
What About Gut Bugs and IBS-U?
We do not have a lot of studies that focus on IBS-U. We do know that the main complaints in IBS-U patients are bloating, gas, and abdominal pain, but not necessarily altered bowel habits. Bloating, gas, and abdominal pain can overlap with any of the intestinal dysbioses listed above (please read above sections), so asking your doctor for a breath test to diagnose would be prudent.
If you’d like to download my IBS-U mini-guide, you can find it here.
Main Takeaways
While it’s true that there are treatments, tips, and tools that might help manage “global” symptoms of IBS, meaning they may prove effective to reduce your symptoms to some extent regardless of your IBS subtype, to experience “next-level” IBS relief, it might be time to layer in tools and strategies specific to your IBS subtype, many of which are noted above.
To experience “next-level” IBS relief, it might be time to layer in tools and strategies specific to your IBS subtype…Symptom-specific IBS management is where it’s at.
The bottom line? Symptom-specific IBS management is where it’s at.
Once you have achieved a diagnosis of IBS (including a subtype) from your medical doctor, work with an IBS-trained Registered Dietitian to ensure you are well equipped with the nutritional tools & tips that might work best for your subtype.

References
Drossman, Douglas.A. “Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features, and Rome IV.” Gastroenterology 150, no 6 (May 2016): 1262–1279.
Lacy, Brian E. PhD, MD, FACG; Pimentel, Mark MD, FACG; Brenner, Darren M. MD, FACG; Chey, William D. MD, FACG; Keefer, Laurie A. PhD; Long, Millie D. MDMPH, FACG (GRADE Methodologist); Moshiree, Baha MD, MSc, FACG. “ACG Clinical Guideline: Management of Irritable Bowel Syndrome.” The American Journal of Gastroenterology 116, no 1 (January 2021): 17-44.
Duker Freuman, T. (2023). Regular: The Ultimate Guide to Taming Unruly Bowels and Achieving Inner Peace. Hachette Go.
“Rome IV Criteria Appendix A: Rome IV Diagnostic Criteria for FGIDs.” Rome Foundation. Accessed April 20, 2023.
Tack, J. & Drossman, Douglas A. “Diagnosing and Treating IBS: Translating Rome IV for GI and Primary Care Teams” (March 2018): Accessed May 1 https://drossmancare.com/download/diagnosis/Diagnosing-and-Treating-IBS.pdf Training course: The Low FODMAP Diet for Irritable Bowel Syndrome. Monash University. Completed March 2022.
Tansel A, Levinthal DJ. Understanding Our Tests: Hydrogen-Methane Breath Testing to Diagnose Small Intestinal Bacterial Overgrowth. Clin Transl Gastroenterol. 2023 Apr 1;14(4):e00567. doi: 10.14309/ctg.0000000000000567. PMID: 36744854; PMCID: PMC10132719.
Shah A, Ghoshal UC, Holtmann GJ. Unravelling the controversy with small intestinal bacterial overgrowth. Curr Opin Gastroenterol. 2023 May 1;39(3):211-218. doi: 10.1097/MOG.0000000000000928. Epub 2023 Mar 1. PMID: 37144539.
Villanueva-Millan MJ, Leite G, Wang J, Morales W, Parodi G, Pimentel ML, Barlow GM, Mathur R, Rezaie A, Sanchez M, Ayyad S, Cohrs D, Chang C, Rashid M, Hosseini A, Fiorentino A, Weitsman S, Chuang B, Chang B, Pichetshote N, Pimentel M. Methanogens and Hydrogen Sulfide Producing Bacteria Guide Distinct Gut Microbe Profiles and Irritable Bowel Syndrome Subtypes. Am J Gastroenterol. 2022 Dec 1;117(12):2055-2066. doi: 10.14309/ajg.0000000000001997. Epub 2022 Sep 6. PMID: 36114762; PMCID: PMC9722381.
Leite G, Rezaie A, Mathur R, Barlow GM, Rashid M, Hosseini A, Wang J, Parodi G, Villanueva-Millan MJ, Sanchez M, Morales W, Weitsman S, Pimentel M; REIMAGINE Study Group. Defining Small Intestinal Bacterial Overgrowth by Culture and High Throughput Sequencing. Clin Gastroenterol Hepatol. 2024 Feb;22(2):259-270. doi: 10.1016/j.cgh.2023.06.001. Epub 2023 Jun 12. PMID: 37315761.
Takakura W, Rezaie A, Chey WD, Wang J, Pimentel M. Symptomatic Response to Antibiotics in Patients With Small Intestinal Bacterial Overgrowth: A Systematic Review and Meta-analysis. J Neurogastroenterol Motil. 2024 Jan 30;30(1):7-16. doi: 10.5056/jnm22187. PMID: 38173154; PMCID: PMC10774808.