Irritable Bowel Syndrome (IBS) is often viewed through the lens of food—especially for anyone familiar with the low FODMAP diet. But what if your symptoms flare even when your diet seems perfectly on track? That’s because IBS isn’t just about digestion; it’s a type of Disorder of Gut-Brain Interaction (DGBI), which means your nervous system plays a major role, too. From stress and sleep habits to environmental changes and even posture, many under-the-radar factors can set off your symptoms. These non-food triggers are real, common, and often overlooked—and understanding them might be the key to finally getting some relief.
Work With A Registered Dietitian

We aren’t saying food doesn’t count. It does! But possibly the single most overlooked component of IBS is non-food triggers. When folks have an IBS flare, we see them go straight to cataloging all the food they have eaten, disregarding the non-food aspects of their everyday lives.
The most efficient and proven way to determine your IBS triggers is to work with a Registered Dietitian. They can help structure the right way for you to approach the low FODMAP diet (strict is not always best), guide you through non-food triggers, and make sure you retain (gain?) a positive relationship with food.
This article takes a look at those non-food triggers that could be wreaking havoc.
Stress and Anxiety—Even the “Good” Kind

This one tops the list for a reason. Stress doesn’t have to be negative to affect your gut. Even joyful life changes—like planning a wedding, starting a new job, or having a baby—can be physically stressful and trigger IBS symptoms. That’s because your nervous system doesn’t always distinguish between “good” stress and bad; it simply reacts. Stress and anxiety influence the gut-brain axis, increasing gut sensitivity and altering motility. According to the American College of Gastroenterology, managing stress through tools like cognitive behavioral therapy (CBT), mindfulness, or yoga can be just as important as diet. Gut-directed hypnotherapy has been shown to be as effective as the low FODMAP diet (we love the NERVA app). If you’re going through a life transition—even a happy one—your gut might be talking louder than usual.
Poor Sleep Habits

You might think a bad night’s sleep just makes you tired and cranky. But for people with IBS, sleep disturbances can actually worsen gut symptoms. A study in Clinical Gastroenterology and Hepatology found that IBS patients who slept poorly reported more severe symptoms the next day. Sleep affects everything from digestion to inflammation to mood—all of which affect IBS. If you’re not sleeping well, your gut is probably suffering too.
Hormonal Changes
Anyone who’s ever had a period or gone through menopause may already suspect this: hormones have a huge impact on digestion. Estrogen and progesterone can influence gut motility and sensitivity. Many people with IBS report symptom flares around their menstrual cycle. And it’s not just female hormones—cortisol (a stress hormone) also plays a big role. That’s why IBS management often requires a look at hormonal balance, especially during puberty, pregnancy, perimenopause, or times of intense stress.
Overexercising or Sedentary Lifestyle

Too much or too little physical activity can both make IBS worse. A sedentary lifestyle can slow digestion and lead to bloating, while excessive or intense exercise can actually trigger symptoms due to increased gut permeability and changes in blood flow. A study published in the American Journal of Gastroenterology found that moderate physical activity, like walking or gentle yoga, helped improve IBS symptoms. So yes, movement helps—but more isn’t always better.
Medications and Supplements

Some common medications can be stealthy IBS triggers. Antibiotics can disrupt gut bacteria, painkillers like NSAIDs may irritate the lining of your gut, and even birth control pills or antidepressants can alter motility. Over-the-counter supplements, including magnesium, iron, and fiber, can also be problematic if not matched to your specific needs, like your IBS-subtype. Always discuss these with a healthcare provider who understands IBS—not all supplements are benign.
Changes in Routine or Travel
Routine might seem boring, but your gut actually loves it. When you travel across time zones, sleep in a new environment, or eat at unusual hours, your digestive system can get thrown off. This is especially true for people with IBS, where even small disruptions in rhythm can cause symptoms. Try sticking to regular sleep and wake times, keeping meals on a schedule, and staying hydrated when traveling.
Temperature Extremes

Hot weather, cold snaps, and sudden temperature changes can all affect people with IBS. For some, heat increases dehydration and causes bloating, while others may experience worsened symptoms in cold environments due to vasoconstriction and tension. While research is still emerging, many people report seasonal symptom flares, especially in high-humidity or very dry conditions.
High-Pressure Work or Toxic Relationships

It’s not just about “stress” in the generic sense—it’s the emotional environment you’re in every day. A job that constantly raises your cortisol levels, or a relationship that makes you feel on edge, can wreak havoc on your digestion. The gut and emotions are so closely linked that some therapists specializing in IBS now include relationship and workplace dynamics in their assessment.
Gut Microbiome Imbalance
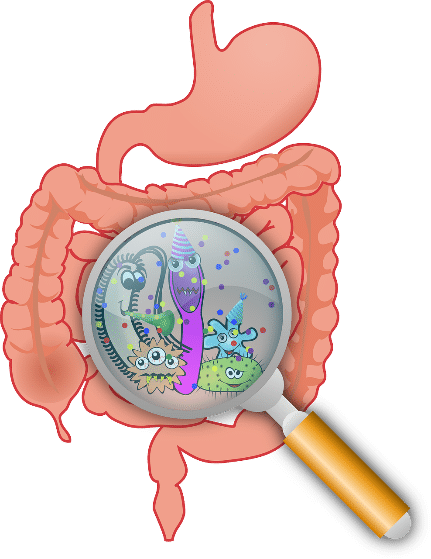
While technically not a food or a feeling, your gut bacteria play a major role in IBS. Dysbiosis—an imbalance in the bacteria living in your intestines—can make the gut more sensitive, alter motility, and trigger bloating and gas. Antibiotic use, illness, stress, or poor diet can disrupt this balance. Probiotics may help—but they need to be chosen wisely, ideally under the guidance of a dietitian or gastroenterologist. There are specific strains of probiotics that are used for specific needs. Probiotics are not recommended during the Elimination of Challenge Phases of the low FODMAP diet, as they alter your digestion of FODMAPs, which is what you are trying to determine at that time.
Pelvic Floor Dysfunction

Pelvic floor dysfunction is one of the most under-recognized non-food causes of IBS symptoms, especially constipation-predominant IBS (IBS-C). The muscles involved in bowel movements may not be coordinating correctly, making it hard to empty completely or leading to a sensation of incomplete evacuation. Pelvic floor physical therapy has helped many people finally find relief where diet failed.
Too Much Gut-Focused Thinking
Ironically, obsessing over your gut can make it worse. Constant monitoring, hyper-awareness of every gurgle, and fear-based food avoidance can reinforce a cycle of anxiety and symptoms. This doesn’t mean your symptoms aren’t real—they absolutely are—but sometimes the psychological feedback loop keeps the IBS fire burning. Techniques like gut-directed hypnotherapy or mindfulness-based stress reduction (MBSR) have been shown to break that cycle effectively.
Chemical Sensitivities and Environmental Irritants

Sometimes it’s not what you eat, but what you breathe in. Strong smells, perfumes, cigarette smoke, cleaning chemicals, or air pollution can be surprising IBS triggers. While more research is needed in this area, anecdotal reports are common. These irritants may activate mast cells in the gut lining, leading to inflammation and hypersensitivity—especially in people who also have conditions like histamine intolerance or multiple chemical sensitivities.
Tight Clothing and Posture

This might sound superficial, but tight waistbands, restrictive clothing, or even slouching can trigger or worsen IBS symptoms like gas and bloating. Compression around the abdominal area can put pressure on the intestines, especially after eating. Good posture, loose clothing, and not lying down immediately after meals can make a noticeable difference for some individuals.
The Takeaway: The Bigger IBS Picture

If you’ve done everything right with your food and still feel miserable, you’re not alone—and you’re not imagining things. Non-food IBS triggers are real, varied, and often under-discussed. Managing IBS requires a comprehensive approach that goes far beyond the plate. Whether it’s stress, sleep, hormones, movement, or emotional wellbeing, looking at the whole picture gives you a far better chance of finding real, lasting relief.