When you hear the term “inner peace” what comes to mind? If you spend your days thinking about bowel habits, it means finding that balance where all is well with your digestive and elimination world.
A good poop calls for sharing the joy with a loved one (we call those “poop friends”; folks you can really talk to about anything). Tamara Duker Freuman MS RD CDN is just that kind of friend and we are here to interview her about her book, Regular, The Ultimate Guide to Taming Unruly Bowels and Achieving Inner Peace.
If you are one of the millions of people worldwide who need insight into their disruptive, and even painful bowel patterns, then this is the book you have been waiting for.

Tamara is an internationally known expert in digestive health and medical nutrition therapy for gastrointestinal diseases, and we are thrilled to be able to bring her right to you. She has authored some of our most popular, and helpful, articles such as Timing of Digestive Symptoms, and Everything You Want to Know About Farting, But Were Afraid To Ask. Her first book, The Bloated Belly Whisperer, should be on your shelf if you deal with bloating on any level. Tamara’s advice is read by hundreds of thousands of people each month through online publications including U.S. News & Health Report, and EatingWell.com.
10 Reasons Why People Suffer From Chronic Diarrhea
Let’s dive into a lively discussion about diarrhea and constipation, why we experience them, and what we can do about it.
Dédé Wilson: Tamara, congratulations on the new book, Regular, The Ultimate Guide to Taming Unruly Bowels and Achieving Inner Peace. Certainly, there is a huge need. We (all of us: you, me, the RDs we work with) spend our days talking to people who have problems with their elimination process (or lack thereof). Talking about poop has come a long way in the last several years. First of all, we have always intellectually understood that everyone poops, but for some reason, it has been (and still is for some) difficult to talk about. But we need to jump into the deep end of the bowl.
Tell us the myriad of reasons why people can have diarrhea and/or be constipated. There are so many more reasons than most of us are aware of.
My book regular covers over ten different reasons why people can suffer from chronic diarrhea. These include functional GI disorders like IBS, which affect the sensory and motor function of the gut. It covers osmotic diarrhea that results from maldigesting certain sugars like lactose, sucrose or fructose. It covers four different malabsorptive conditions, including bile acid malabsorption, small intestinal bacterial overgrowth (SIBO), celiac disease and pancreatic insufficiency. It covers inflammatory bowel diseases like Crohn’s disease and ulcerative colitis, and it also covers histamine intolerance, which is a lesser-known condition that results in swelling in the bowel that can result in diarrhea in predisposed people.
As far as constipation goes, I also cover a few different causes including slow motility and, once again, functional GI disorders like IBS. I cover ‘normal transit constipation’ which may be aggravated by lack of dietary fiber or just an imbalance of dietary fiber types, which we see a lot with people who follow very low carb or keto diets, or other types of extreme elimination diets. The book also covers pelvic floor dysfunction, which is a neuromuscular issue that can impact your ability to empty your bowels completely or adequately.
What prompted the writing of the book? What are the statistics? How many of us are experiencing bowel habit issues? And how are they defined as a problem? Also please touch on why it is important that one addresses these issues.
After my first book, The Bloated Belly Whisperer, it became clear to me that not all people with GI problems were going to find answers to their problems in my book. People were messaging me online asking me if my book covered conditions like IBS or Crohn’s disease, and in reality, there were aspects of these conditions that my book covered, but it didn’t really offer a comprehensive guide to managing a lot of medical diagnoses– and specifically to managing chronic diarrhea.
I realized there was probably another book in me that could really specifically address the issues of the many causes of diarrhea and the many causes of constipation and be a comprehensive management resource for people specifically struggle with bowel regularity, which is easily one-third of all Americans.
What Can You Do About It?
So, now we know all the reasons why we might experience unruly bowels, but the million-dollar question, of course, is what can we do about it? As each of us is unique, with a unique digestive track, it is never one size fits all, is it?
Treating bowel irregularity completely depends on the cause for your irregularity, and the whole point of this book is to really help readers pinpoint the cause of their problem so they know how best to solve it. Someone having diarrhea because they malabsorb fructose has a really different solution then someone who has chronic diarrhea because of histamine intolerance or ulcerative colitis.
Someone who’s constipated because they don’t eat enough fiber has a really different solution then someone who’s constipated because they have pelvic floor dysfunction; in fact, people with pelvic floor dysfunction often feel worse when they eat high fiber diet as compared to someone who has IBS-C who may do a bit better on a higher fiber diet.
The devil is in the details when it comes to managing unruly bowels. You really need to understand what is going on with you physiologically so that you can tailor a solution that’s targeted to the problem, whether it’s a diet change, a supplement regimen, medications or behavioral health interventions.
If you want to learn more about Fructose Malabsorption watch our video:
The devil is in the details when it comes to managing unruly bowels. You really need to understand what is going on with you physiologically so that you can tailor a solution that’s targeted to the problem, whether it’s a diet change, a supplement regimen, medications or behavioral health interventions.
Using A Diagnostic Tool In The Book
Very early in the book you lay out a diagnostic tool that you have developed, with the intention of the book being a self-help tool. This will be a very popular aspect of the book, I am sure. Tell us how this works, and how you determined that people could use this tool without making incorrect assumptions and choices.
When I first meet with a patient, I have them take me through a typical day in their life, including their usual symptom patterns. I’m asking very pointed, very specific and very differentiating questions so that I can quickly develop a hypothesis about what may be going on with my patient. Then, I can test my hypothesis with a particular diet intervention or other type of remedy so see if my patient responds.
The quizzes that I’ve developed in both of my books along with my gastroenterologist colleague, Dr. Eric Goldstein, really attempts to mimic the in person “Q&A” that GI dietitians or gastroenterologists might engage in as we attempt to develop hypotheses around what’s going on with our patients.
Once you complete the quiz in my books, your score will direct you to a chapter or chapters that seem to correspond most closely with your answers. You can then read that chapter and see if the description of the symptoms and the conditions really resonates with you so that you can then have your own hypothesis about what could be going on with you, and test out the diet or the remedies that I suggest–or have an informed conversation with your doctor about whether they feel the hypothesis would be worth investigating medically.
The way I road-tested this quiz was by consulting the medical charts of many of my patients and filling out the quiz based on information that they provided to me in our first session. I then scored up the quiz and compared the answer that the quiz produced against what my patient was ultimately diagnosed with, to see whether the quiz was generally on point.
I’ll also say that the quiz from my first book, The Bloated Belly Whisperer, has been in circulation for over five years at this point, and I’ve gotten feedback from hundreds of people that the quiz been markedly effective at helping them narrow down a possible medical diagnosis that they were then able to go to their doctor and get tested or treated for.
I do think it’s important to mention that even though this quiz does mimic the diagnostic process that we undergo in our practice, neither me nor Dr. Goldstein are diagnosing readers of this book; you really need to get a medical diagnosis from your own physician and cannot self-diagnose on the basis of the educated guesses that my books’ quizzes offer.
…you really need to get a medical diagnosis from your own physician and cannot self-diagnose on the basis of the educated guesses…
How To Get Properly Diagnosed
You mention some people in the book who have had issues that were misdiagnosed, which of course lead to improper treatment. Please lay out the best approach for someone who is looking for an accurate diagnosis. What should they do, where do they look? How can one know that they are being accurately diagnosed?
The best way to know if you’ve been accurately diagnosed is if you’ve actually responded to the treatments and/or the diets that are typically effective for people with that diagnosis. If you’ve been diagnosed with IBS and you have tried four or five different IBS medications, the low FODMAP diet or fiber therapy—in other words, a variety of evidence-based remedies that usually have some impact for people with IBS–and you haven’t responded at all to any of them, that’s when I think you need to start questioning whether you’ve actually been accurately diagnosed.
Similarly, if you’ve been diagnosed with celiac disease and you’re following a strict gluten free diet and your celiac disease antibodies are clear and your endoscopies show that the disease is quiescent, but you’re still extremely symptomatic, we have to start looking elsewhere.
Maybe it’s not just the celiac disease that’s been causing your symptoms, but perhaps there is a comorbidity that is also at play and we should be digging deeper. Same with Crohn’s disease; if your disease is in remission and you’re still very symptomatic, we need to be evaluating whether there is something else going on in addition.
Keeping detailed notes about your observations regarding your symptoms is a great place to start; my patients usually have all the clues I need in order to develop a hypothesis about the origin of their ongoing symptoms. You may not know how to make sense of these clues, but that’s where an experienced GI- focused registered dietitian or your doctor can really help connect the dots and figure out what could be going on.
Check out this symptom journal here.
If you keep getting told that you have IBS and you’re not responding to anything that your doctor prescribes, I think it’s perfectly appropriate to ask your doctor: ‘Are there conditions that may look like IBS but that are actually not IBS? What might some of those conditions be, and how would we figure out if I have one of those?’ I call these conditions “IBS mimickers,” and a several of them are covered in REGULAR.

Allergies vs Intolerances: Setting The Record Straight
Can you please address food sensitivity testing, particularly tools that are accessible at home, and also discuss the differences between intolerances and allergies? One of the most challenging aspects of my days are when I encounter folks in our Facebook groups who announce that they are allergic to XYZ, PD&Q. They will list several things. We have no idea how these were diagnosed, and the terms “allergy” and “intolerance” are most often used interchangeably. I am often concerned that people are misdiagnosed (self or otherwise) and therefore over-restricting, yet one doesn’t want to invalidate folk’s experiences. I know there is a lot to unpack here, but you do address food sensitivity testing in the book, so perhaps start there, and also discuss the differences between allergies and intolerances.
Food allergies are adverse food reactions carried out by your immune system. Typical food allergy is mediated by IgE antibodies, but there are also atypical food allergies that are carried out by white blood cells called eosinophils, and these reactions are typically limited to the GI tract—the esophagus, stomach or intestine.
Eosinophilic food reactions do not generally show up in standard food allergy tests, like bloodwork or skin prick tests; they are diagnosed with biopsies of the GI tract and their response to elimination diets and rechallenges; it’s a pretty intense diagnostic process, which means these conditions are often underdiagnosed.
Food intolerances are not carried out by the immune system. These are adverse reactions more likely related to maldigestion, malabsorption or chemical sensitivities to compounds in food. While we have breath tests and/or small bowel biopsies that can diagnose malabsorption of sugars like lactose, sucrose and fructose, there are no other scientifically validated tests for food intolerance or ‘food sensitivity.’
The so-called ‘food sensitivity’ tests that are marketed directly to consumers or ordered by alternative medicine providers are not scientifically validated or evidence based.
The so-called ‘food sensitivity’ tests that are marketed directly to consumers or ordered by alternative medicine providers are not scientifically validated or evidence based.
These are tests that are using immune system markers that have not been demonstrated to be diagnostic of food sensitivity as indicators of food sensitivity—or, tests that tell consumers that their lab values mean something that they do not.
This typically leads to extremely widespread elimination diets, a lot of food fears and food anxiety without really offering very specific insight into the something that is actually bothering you.
If there is a food in your habitual diet that is bothering you, chances are that it will get swept up in a wholesale elimination diet that has you removing 50% of what you typically eat. But not all GI symptoms are due to a specific food intolerance or sensitivity, and the assumption that all of your GI problems are caused by a specific food is erroneous and leads to excessive reliance on elimination diets.
But not all GI symptoms are due to a specific food intolerance or sensitivity, and the assumption that all of your GI problems are caused by a specific food is erroneous and leads to excessive reliance on elimination diets.
The most common problem I see in practice is people who are bloated, gassy and experiencing abdominal pain because they are completely full of stool—just utterly backed up. In these cases, elimination diets are useless. The problem is too much fiber, period. You’re not going to be able to isolate or pinpoint a specific food trigger because the problem isn’t being caused by a specific food, but rather by an entire dietary pattern.
What About SIBO?
SIBO is a hot topic of discussion in our community. Take us through the current science of diagnosis and treatment, and please touch on methane overgrowth.
Small intestinal bacterial overgrowth (SIBO) is diagnosed via breath testing even as experts acknowledge that breath testing isn’t 100% accurate, and there can be false negatives and false positives.
Breath testing allows us to see whether someone is overgrowing microorganisms in their small bowel and also what type of microorganisms they are overgrowing– whether hydrogen producing or methane producing– so that doctors can tailor a course of antibiotic treatment that is most likely to be effective.
When physicians forego breath testing and just treat empirically with antibiotics based on a hunch, there is a risk that the medication chosen may not be well-suited to eradicate methane-producing organisms. In these cases, a lack of response to treatment is often be misconstrued as “well, I guess you didn’t have SIBO after all” and people with methane-predominant SIBO go undiagnosed and untreated.
There is some new technology currently under development that promises more accurate SIBO diagnostics through a swallowable capsule that analyzes intestinal fluid and can quantify bacterial loads. If and when this capsule comes to market, I hope we will see increased access to and confidence in SIBO diagnostics.
SIBO is a condition that does have a high recurrence rate, and often that’s because the conditions that allowed somebody to overgrow bacteria in their small intestine need to be identified and remedied if you are to prevent that overgrowth from recurring.
Unfortunately, not all patients with SIBO are getting more comprehensive evaluation to identify their predisposing factor, so we do see a very frustrating recurrence rate of SIBO among people for whom it might actually be preventable. In our practice, patients with recurrent SIBO are generally getting some systematic evaluation and diagnostic testing by their gastroenterologist to see if we can identify some of the more common reasons and rectify them. Certainly, though, there are some people with unmodifiable risk factors for whom SIBO is unfortunately going to be more of an ongoing, recurrent problem.
You May Want To Read: SIBO: Get The Facts
Currently there is no good scientific evidence that over-the-counter or herbal remedies are an effective treatment for SIBO; the idea of ‘herbal antimicrobials’ has been way oversold in the alternative medicine cottage industry that has emerged around SIBO treatment.
In reality, none of these herbal compounds has demonstrated anti-microbial benefits in vivo and none of these elaborate supplement protocols have demonstrated statistically significant efficacy in SIBO eradication alone or in comparison to the standard dose of antibiotic treatments in current circulation.
There is also no good evidence to suggest that specific foods or diets can cause, eradicate or prevent SIBO, nor is there any good evidence that probiotic supplements can help treat or prevent SIBO. It pains me as a dietitian to have to admit the limited role of diet in anything other than symptom management when it comes to SIBO.
I wish I had more optimistic news here, but I’ve seen hundreds if not thousands of patients be misled by false promises about what causes, prevents and treats SIBO, spending hundreds of dollars if not more on unproven, unscientific and extremely expensive protocols.
Let’s Talk About Histamine Intolerance
Chapter 8 focuses on histamine intolerance, which is something we are hearing more about. This is a complex issue; can you give us the snapshot of proper diagnosis and treatment, and it relates to certain elimination patterns?
Histamine is a signaling molecule that the body produces for a variety of functions. Notably, it plays a role in stomach acid release and also in the allergic response. Histamine is the reason why your mosquito bites swell up or you may have itchy eyes in response to seasonal allergens. Histamine also exists naturally in some foods, or can be created as a byproduct of food aging, curing, fermentation and spoilage.
Because a buildup of histamine can cause allergic type symptoms or GI symptoms, the body needs a mechanism to break down excess histamine so that it doesn’t build up. That mechanism is largely the job of an enzyme called DAO (diamine oxidase) which breaks down histamine in our body.
If your white blood cells produce a lot of histamine (such as during allergy season) or you consume a lot of histamine from your diet and you don’t make a lot of DAO (or enough DAO) to break it down fast, enough the histamine buildup can produce symptoms throughout the body including in the GI tract, but certainly not limited to it. The symptoms can include acid reflux or indigestion, bloating, diarrhea or abdominal pain, but also rashes, hives, rapid heartbeat or an anxious feeling, brain fog or headaches.
There is no validated way yet to diagnose histamine intolerance, so generally the diagnosis is made based on symptoms that are provoked by high histamine foods, and/or symptoms that improve when following a low histamine diet, using a DAO enzyme supplement and/or antihistamine medications.
How Pelvic Floor Dysfunction Affects Your Bowels
Ditto with pelvic floor dysfunction; this is coming up more in articles and conversations and most of us do not know what it is, or how it affects the bowels. We look to you for a brief intro.
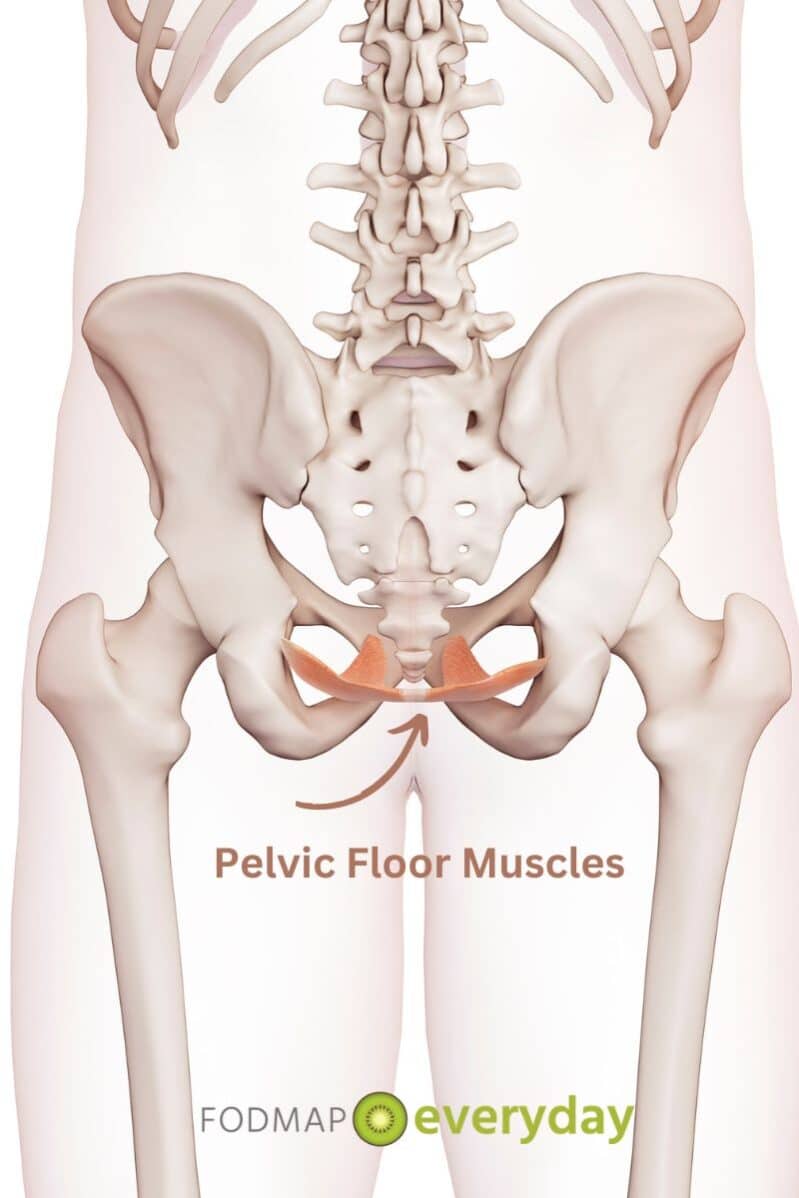
There are a series of muscles that comprise the so-called “pelvic floor.” A fitness instructor I know, Manuel Velazquez, once jokingly described these muscles as being responsible for ‘holding in or releasing liquids, solids and gasses,’ and I think that’s a pretty terrific summary.
The pelvic floor muscles must coordinate in a specific way in order to allow us to move our bowels completely or easily, to urinate and even to experience painless sexual activity, so when one or more of these muscles is not functioning properly, we can experience problems with pooping, peeing or vaginal/anal sexual intercourse. Muscles may be too tight, too weak, or they just may not be coordinating properly to allow for normal function along any of these dimensions.
Pelvic floor dysfunction is a really under-recognized cause of bowel issues, particularly chronic constipation, but also fecal incontinence. It’s estimated that 40% or more of people who are chronically constipated may actually have some form of pelvic floor dysfunction. PFD can affect both women and men, but women over the age of 40 are particularly susceptible.
Our Lightening Round Of Questions For Tamara!
This interview really could go on and on. The book is over 300 pages, and of course, each of the topics we have touched upon are delved into much more deeply. When the reader works through the diagnostic tool, they are then directed to the exact parts of the book that are applicable to them. It is laid out brilliantly! Kudos to you and your editor. I know you said you only expect your Mom to read the whole thing, but it is actually a truly illuminating read.
Let’s end with a lightening round:
1. What is the biggest issue you see in your clinical practice in terms of elimination problems?
I estimate that about 40% of the patients I see are actually completely “FOS” (which stands for ‘full of stool’). This can happen even to people who go to the bathroom every day, or even who go to the bathroom multiple times per day if their dietary fiber intake far exceeds the amount of stool that they’re able to eliminate.
These patients of mine often present as incredibly bloated—not too bad in the morning but it builds as the day progresses—and feel worst at night with bloating and extremely gassiness no matter what they’ve eaten.
2. What is the #1 reason you see holding people back from receiving an accurate diagnosis?
Doctor visits that are too short, complicated by the fact that my patients don’t always have the language to describe precisely what they’re experiencing. When you have a very short amount of time for a conversation with your doctor AND you’re not able to clearly explain what you’re experiencing, a lot of assumptions can be made that aren’t necessarily true. This can obfuscate the diagnostic process.
For example, a patient may say ‘I’m really bloated,’ and doesn’t really know that “bloating” may mean something different to them than it does to their physician. Perhaps the doctor will make an assumption about what ‘bloating’ means– maybe to them, it implies indigestion or acid reflux, so the patient is prescribed an antacid medication or maybe even an upper endoscopy will be ordered. But in reality, the patient may be referring to a lower abdominal bloating that has to do with constipation, so the antacid is going to do nothing for you and an upper endoscopy will be unrevealing.
The advantage I have as a dietitian is that I spend between 30 and 60 minutes with a patient. I have the luxury of time to really probe and dig deep and get a lot of details about a patient’s subjective experience, their diet and the interplay between their symptoms and their food choices or eating patterns. This allows me to see a fuller picture then some of my physician colleagues have the luxury of obtaining in a 10-to-15-minute visit.
This is why I think it’s so important for patients to come prepared to their doctor visits, and why in my books I try to equip people with more precise language and descriptions that they can convey to their own providers so as to facilitate the diagnostic process.
3. Once a diagnosis is made, what are the biggest obstacles you see for people when it comes to following through on a treatment plan and achieving their bowel goals?
I think there’s a lot of “all or nothing” or “black and white” thinking when it comes to diet and nutrition in general. It’s hard enough to change any habit to begin with, and anyone who attempts to undertake an extreme and rapid change in terms of how they eat, what they eat or with exercise, often finds it really hard to sustain.
So after about a week or two of really focused effort, you completely give up and wind up not doing anything different at all. When in reality, people typically benefit from taking on a change even someof the time or most of the time; you don’t have to be perfect to make progress, and I think extremes in thinking and extremes in eating are rarely sustainable. They’re also rarely necessary to get results.
Tamara, thank you for all you do for those of us dealing with these life-affecting gastrointestinal issues. You have truly changed and saved lives!
Grab your copy of Tamara’s Book here.
Read All Of Tamara’s Articles:
- What Conventional Wisdom Gets Wrong About Bloating
- Timing of Digestive Symptoms: What It Means
- What Is Leaky Gut Syndrome?
- Are You Full of Sh*t? Stool Burden and the Low FODMAP Diet
- Everything You Want to Know About Farting*
- 5 Reasons to Skip Gut Microbiome Testing – For Now
- Exclusive Interview with Dietitian Tamara Duker Freuman
- Q & A With The Author Of “Regular, The Ultimate Guide to Taming Unruly Bowels and Achieving Inner Peace”