Irritable Bowel Syndrome (IBS) and autoimmune diseases are distinct medical conditions that can significantly impact an individual’s quality of life. While IBS is characterized by chronic gastrointestinal symptoms, autoimmune diseases involve the immune system mistakenly attacking the body’s own cells. The intersection of these two conditions is a complex and evolving area of medical research, with emerging evidence suggesting potential links between them.
IBS: The Gut-Brain Connection
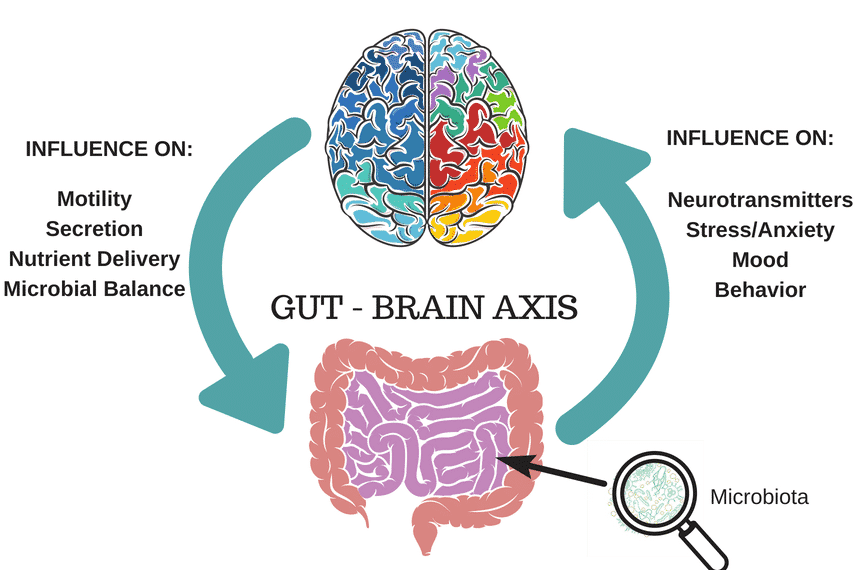
IBS is a common disorder affecting the large intestine, leading to symptoms such as abdominal pain, bloating, gas, diarrhea, and constipation. It is referred to as a DGBI, which stands for “disorder of gut-brain interaction”.
Unlike inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis, IBS does not cause visible inflammation or damage to the digestive tract. The diagnosis of IBS is typically made based on symptom patterns put forth by the Rome IV criteria, and by ruling out other conditions, such as celiac, diverticulitis, endometriosis, and other conditions.
However, there is increasing evidence that low-grade inflammation and hyper-permeability of the intestinal barrier are often present in individuals with IBS, even though these issues do not appear on routine tests like colonoscopies. While IBS is currently recognized as a gut-brain disorder, this evidence suggests that additional factors may be involved (and we may even see a change in its definition in the future).
Autoimmune Diseases: Systemic Immune Response

Autoimmune diseases are characterized by an inappropriate immune response against healthy tissues. There are over 100 recognized autoimmune diseases, each affecting different organs or systems in the body. Common autoimmune diseases include rheumatoid arthritis, lupus, and multiple sclerosis. These conditions can cause a range of symptoms, depending on the tissues targeted by the immune system.
The Potential Link Between IBS and Autoimmune Diseases

Recent research has begun to explore the relationship between IBS and autoimmune diseases. While IBS is not classified as an autoimmune disease, studies have found that individuals with autoimmune conditions may have a higher prevalence of IBS symptoms. This suggests that there may be shared mechanisms or that the presence of an autoimmune disease could predispose someone to develop IBS.
Some studies have found evidence of low-grade inflammation and immune activation in the intestines of IBS patients, although this is not a defining characteristic of IBS.
Immune System Dysfunction

One hypothesis for the connection between IBS and autoimmune diseases is immune system dysfunction. In autoimmune diseases, the immune system erroneously targets healthy cells, leading to inflammation and tissue damage. Similarly, some studies have found evidence of low-grade inflammation and immune activation in the intestines of IBS patients, although this is not a defining characteristic of IBS.
It seems there is not a clear conclusion on whether chronic inflammation is always present, but we can hypothesize a connection. Dysbiosis, defined as an imbalance in the gut microbiome, has been linked with IBS, and microbial dysbiosis has been shown to drive auto-immune conditions and local inflammatory conditions like diabetes and inflammatory bowel disease.

A systematic review from 2022 showed most studies included concluded that IBS patients have a reduction in bacterial diversity and less stability of the microbiota. The review concluded that the gut microbiome plays a substantial role in the development of IBS.
So how does dysbiosis lead to inflammation and contribute to IBS? Dysbiosis can lead to degradation of the intestinal epithelium mucosal layer, also known as intestinal hyperpermeability or “leaky gut”. In those with IBS-D, elevated inflammatory markers were found in one study.
For more information on “leaky gut”, and why we have that term in parentheses, please refer to our article: What Is Leaky Gut Syndrome?

In terms of specific bacteria strains, Bifidobacterium – which play a role in maintaining the mucous layer of the intestinal barrier amongst other health benefits – has been shown to be reduced in those with IBS. We have also seen that a low FODMAP diet is linked with reduced levels of Bifidobacterium, although it’s not clear for how long or the quality of the diet followed.
If you have not yet heard of Mark Pimentel and his research lab at Cedars-Sinai, here’s why you should. They have been spearheading research on IBS, SIBO and the microbiome for the last 20 years and have developed a test that can diagnose IBS-D and IBS-M known as IBS-SMART. (Please note that it does not include IBS-C. Here is an article on IBS Subtypes; your sub-type should determine treatment).
The test measures the blood levels of validated IBS biomarkers anti-CdtB and anti-vinculin, which are thought to develop after a case of food poisoning, leading to microbiome disruption. They have been shown to be elevated in a majority of IBS patients with diarrheal symptoms, and can diagnose diarrhea-predominant or mixed-type IBS (IBS-D or IBS-M).
Anti-vinculin is an autoimmune response against a protein, vinculin, that is considered critical for healthy gut function. Elevated levels of either of these antibodies can indicate IBS, according to Pimentel. This can essentially explain an immune system reaction as a result of food poisoning, leading to IBS development. While these tests can replace unnecessary invasive testing like scopes as they distinguish between IBS and IBD, they are not yet in common practice. As well, these biomarkers are not commonly elevated in constipation-predominant IBS (IBS-C).
Shared Genetic and Environmental Factors

Both IBS and autoimmune diseases may share common genetic predispositions and environmental triggers. For instance, stress and infections have been implicated in the onset of both types of conditions. Additionally, a family history of autoimmune diseases may increase the risk of IBS, suggesting a potential genetic link.
While there are not currently any systematic reviews or meta analyses (aka high level research papers looking at multiple studies on the same topic), there are some studies including twin studies which suggest a genetic link with IBS. It should be noted that when it comes to genetics, our environment, diet and lifestyle factors can play a role in “turning on” or “turning off” our genes, aka “epigenetics”.Therefore, having a family history of IBS does not guarantee you will develop it per se. However, exposure to known IBS risk factors such as food poisoning, a Western-style diet (low fiber, high saturated fats), or high stress may increase your likelihood of developing IBS as a result.

You May Want To Read: Is There a Link Between Being a ‘Good Girl’ and Autoimmune Disease in Women?
Overlapping Symptoms

Symptoms of IBS can overlap with those of autoimmune diseases affecting the gastrointestinal tract, such as IBD. This can make diagnosis challenging, as it is essential to distinguish between functional symptoms of IBS and the systemic inflammation seen in autoimmune diseases.
Diagnostic Challenges and Considerations

Diagnosing IBS in the presence of an autoimmune disease requires careful evaluation to rule out other conditions that could explain the symptoms. Physicians may use a combination of medical history, physical examination, blood tests, stool tests, and endoscopic procedures to differentiate between IBS and autoimmune diseases. It is also possible to have both IBS and IBD.
Treatment Implications

The potential overlap between IBS and autoimmune diseases has implications for treatment. For autoimmune diseases, immunosuppressive medications are often used to control the immune response. In contrast, IBS treatments focus on symptom management through dietary changes, stress reduction, and medications to regulate bowel function.
Future Research Directions

Further research is needed to fully understand the relationship between IBS and autoimmune diseases. Studies are exploring the role of the gut microbiome, immune system markers, and genetic factors in both conditions. This research may lead to new diagnostic tools and treatments that address the underlying mechanisms shared by IBS and autoimmune diseases. As an example, identifying inflammatory markers in IBS subtypes may help with targeted therapy.
As mentioned earlier, the IBS-SMART test can detect specific antibodies that indicate an imbalance in the gut microbiome in IBS-D and IBS-M. This information may currently support targeted microbiome therapies. Pimentel Lab is actively researching this area, and we are excited about the potential for improved IBS treatments based on underlying causes!
The Takeaway

While IBS is not an autoimmune disease, there is a growing body of evidence suggesting a complex relationship between these two conditions. The intersection of IBS and autoimmune diseases is an area of active research, with the potential to improve our understanding of both conditions and lead to better patient outcomes. As our knowledge expands, it is likely that the approach to diagnosing and treating IBS in individuals with autoimmune diseases will continue to evolve.