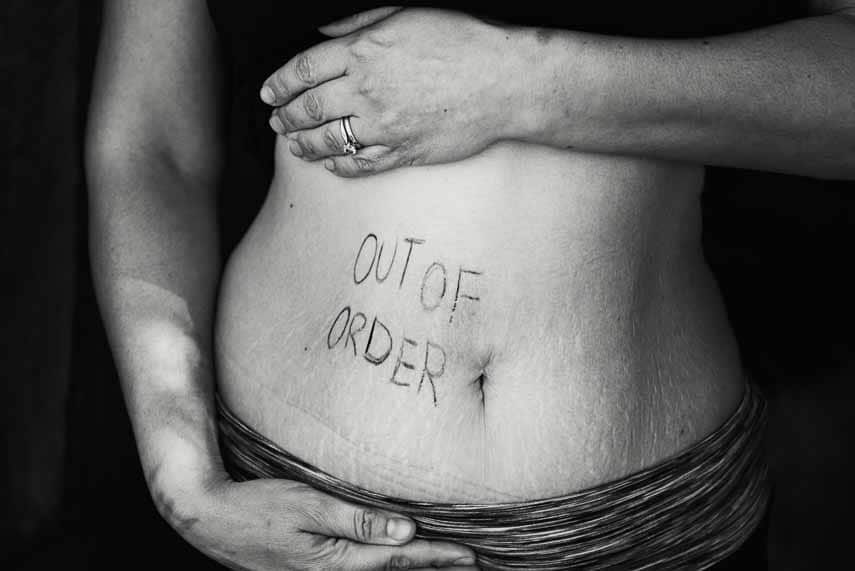
Welcome to the realm of irritable bowel syndrome (IBS), a prevalent and chronic disorder that affects over 1 billion individuals worldwide. Despite its widespread occurrence, IBS is far from a one-size-fits-all condition. Each person’s experience with IBS is distinct, with a unique set of symptoms and challenges.
In this exploration of IBS, we will shed light on the intricacies of its diagnosis, delve into effective symptom management strategies, and ultimately uncover valuable takeaways to empower those navigating this condition. Whether you’re a patient seeking understanding or a caregiver offering support, this comprehensive guide to IBS will provide valuable insights for everyone involved.
IBS Explained
IBS is a chronic digestive disorder affecting the large intestine with no known cause and cannot be cured. IBS manifests in various forms, including abdominal pain, extreme bloating, diarrhea (IBS-D), constipation (IBS-C), alternating episodes of both (IBS-M), or IBS-U (Unclassified) where symptoms may vary. Changes in bowel habits and movements are often indicative, and not all individuals with IBS will exhibit the full range of symptoms.
Please read our article: IBS Subtypes: Your Specific Type of Irritable Bowel Syndrome Will Determine Treatment.
IBS is classified as a “functional gastrointestinal disorder” and is now commonly referred to as a gut-brain interaction disorder. It is distinct from conditions such as ulcerative colitis, colon cancer, Crohn’s disease, or inflammatory bowel disease (IBD).
Learn more in our article, What Is IBS?
The symptoms of IBS stem from abnormal intestinal motility, which can either be too fast leading to diarrhea, or too slow resulting in constipation. Increased sensitivity to pain (visceral hypersensitivity) and a condition known as “high stool burden” also contribute to the symptoms. Bloating, gassiness, bowel urgency, and the presence of mucus in the stool are commonly experienced in IBS cases. Additionally, weight loss or weight gain can be associated with IBS.
A proper IBS diagnosis must be made before the right approach to your treatment can commence…it is often a Registered Dietitian (RD) who helps determine your IBS subtype.
IBS Diagnosis

IBS is not a life-threatening condition, although it can be debilitating and disrupt your life, including your ability to eat, work and socialize normally. It can also mimic other medical issues, which are potentially deadly. It is vital that you get an accurate diagnosis from a medical doctor.
It is tempting to look up symptoms and self-diagnose, but a proper IBS diagnosis must be made before the right approach to your treatment can commence.
A gastroenterologist, or possibly as general practitioner, can diagnose your IBS. A Registered Dietitian (RD), or equivalent in your country, can then help design and implement the right approach of treatment for you, which might include the low FODMAP diet.
When working with your gastroenterologist, make sure you receive a clear understanding of what kind of IBS you have. There are the 4 subtypes, mentioned above, and proper treatment will greatly depend on what kind you have. If your MD has not been this specific, it is time for you to ask more questions and/or get another diagnosis. Practically speaking, it is often a Registered Dietitian (RD) who helps determine your IBS subtype.

IBS Symptom Management
While there is no cure for IBS, there are many successful ways to manage symptoms. Between diet, lifestyle changes, medications, supplements, and psychological support, there are many approaches that a medical doctor and dietitian can choose from to build your unique IBS toolbox. What your IBS treatment plan looks like will be unique to you.
The Low FODMAP Diet for IBS & Other Treatments
The low FODMAP diet is an extremely effective tool for managing IBS symptoms. About 75% of those with IBS respond favorably to the diet, but the implementation is key.
First of all, the developers of the low FODMAP diet always intended the diet to be undertaken along with a RD, although many doctors are not sharing this information. We believe this is possibly the biggest oversight in relation to the low FODMAP diet. Anecdotally and statistically IBS patients will have better management of symptoms if they work with a RD, in addition to saving time and money.
We know many patients will be paying out of pocket for a dietitian, but again to reiterate, if you work with one from the beginning, you will save money and time.
The right approach to the diet will be different for every person. This is also why asking people on social media about their approach is folly. A dietitian will consider your entire medical presentation and your lifestyle. Here are aspects to be considered:
- Other medical issues, such as diabetes, IBD, anxiety, depression, eating disorders, hormonal status, to name just a few.
- Additional digestive issues such as GERD, SIBO, gall bladder disease, and/or exocrine pancreatic insufficiency, for instance.
- The patient’s age. If the patient is a child, it is strongly recommended that a pediatric dietitian be engaged.
- Lifestyle:
- Don’t like to cook, or don’t know how
- Only cook from scratch
- Live in a dorm with no kitchen
- Eat out a lot
- Smoker
- Drink a lot of caffeine
- Frequent alcohol consumption
- Exercise regime, or lack thereof
- Sleep patterns
Depending on all the above, and more, established during discovery with your dietitian, they will tailor the diet to your specific needs. For instance, there is a Gentle Low FODMAP Diet approach, which is appropriate for many patients, and, depending on whether you are IBS-D, IBS-C, IBS-M, or IBS-U, recommendations will vary. What is right for the IBS-D patient is not going to work for those with IBS-C and could actually make things worse.
Medications & Supplements

If you have been taking medications or supplements, it may be proper for you to continue or discontinue them. In addition, new medications and /or supplements might be suggested upon IBS diagnosis.
This is another area where your gastroenterologist and your FODMAP trained dietitian should be working closely together. Here are some examples as to why:
- Do you have additional medical issues that requires medication? Discuss with your doctor about any possible gastroenterological side effects that could be occurring with your medication. Is the medication necessary? Are there alternatives with fewer digestive triggers?
- Are you taking a medication or supplement that specifically triggers IBS symptoms in your IBS subtype? If you have IBS-C and take a medication that has constipation as a side effect, this should be taken into consideration.
- Did you know that you are not supposed to take probiotics or digestive enzymes during the Elimination or Challenge phases of the low FODMAP diet? This is because they can alter your digestion of FODMAPs, which is exactly what you are trying to assess during that time. This is a perfect example of something that a FODMAP trained dietitian would be aware of, but a gastroenterologist or general practitioner would not be (we see this all the time).
- The above bullet point goes for any type of medication or supplement. Your medical doctor might suggest an anti-spasmodic, for instance, but taking one could cloud your assessment of your tolerance to FODMAPs. We are not suggesting that you stop taking a recommended medication. We are making a point about why it is imperative to educate yourself, ask questions, and to work with a FODMAP trained dietitian who best understands how to implement the diet for you specifically in order to have success in minimizing or eliminating IBS triggers.
Lifestyle Changes: Supporting Your Mind
Many people diagnosed with IBS assume that the foods they eat are their main IBS triggers. While food certainly plays a role, there are many other potential triggers and treatments to consider.
Hopefully most of you know by now that proper exercise, general nutrition, and sleep are vital to good health. Even so, most people think about the physical benefits of these important factors, when the mental component is just as important.
We have articles for you on proper sleep patterns, and exercise, but let’s look at the gut-directed hypnotherapy, which has been clinically proven to help with IBS triggers.
Gut-directed hypnotherapy, such as the program that Nerva has developed, have been shown to work as effectively as the low FODMAP diet in the treatment of IBS symptoms [1]. Because IBS is a gut-brain interaction disorder, this makes total sense, and easy to explain.
Gut-Directed Hypnotherapy Is Clinically Proven

As a gut-brain axis disorder, IBS is a two-way street. What happens in the mind can affect the gut, and vice versa. Most of us can identify with the sensation of experiencing “stomach butterflies” when stressed, or excited. This is an example of how the mind connects to our gut. On the other side of the coin, when we feel physical pain, emotional turmoil can result.
Gut-directed hypnotherapy, known as GDH, has been shown to significantly improve gut symptoms such as pain, stool consistency, bloating, distension, gassiness, and nausea.
Dr. Simone Peters is part of Monash University and the founder of Mind + Gut Clinic, which specializes in gut-directed hypnotherapy. Even though Monash University researchers developed the low FODMAP diet, they are proponents of this approach to helping IBS patients.
Dr. Peters has worked with the developers of Nerva, which is app based. It is a gut-directed hypnotherapy program that you can do on your own. It has been quite successful for many IBS sufferers.
Everyone’s IBS presents differently, and successful treatment will be customized to the patient’s unique needs... crowd-sourcing information online and on social media is a bad idea and could make symptoms worse.
The Takeaway

IBS is a debilitating condition that affects over 1 billion people worldwide. While there is no known cure, there are many ways to treat your IBS in order to greatly reduce, and even eliminate, symptoms.
The key is an accurate diagnosis from a medical doctor and to work along with a Registered Dietitian, or the equivalent in your country. Do not self-diagnose. There are life-threatening medical issues that mimic IBS. Your medical team – MD and RD – will devise a treatment plan that is specific for you.
Everyone’s IBS presents differently, and successful treatment will be customized to the patient’s unique needs. This is why trying to self-diagnose and create an approach to your IBS by crowd-sourcing information online and on social media is a bad idea and could make symptoms worse.
The great news is that there are many ways to approach IBS; there is a way for you to experience relief, if you follow our guidelines.
Be sure to check out our articles, which provide more information on topics covered in this post:
- What Is IBS?
- The Gut-Brain Connection & IBS: It’s Not All in Your Head
- The Low FODMAP Diet
- The Role Of The Dietitian vs. The Gastroenterologist
- How to Choose a Dietitian
- Dietitians & Nutritionists: What’s the Difference?
- How Does Sleep Impact IBS?
- Chrono-nutrition, Circadian Rhythms & Irritable Bowel Syndrome
- How to Avoid Gastrointestinal Issues During Exercise
- Pre-Workout Nutrition And The Low FODMAP Diet
- Post-Workout Nutrition And The Low FODMAP Diet
- Gut Directed Hypnotherapy: Promising Therapy for IBS
- Meet Nerva: The Science Backed App For Managing IBS With Hypnotherapy
References
1. S L Peters, C K Yao, H Philpott, G W Yelland, J G Muir, P R Gibson. Randomised clinical trial: the efficacy of gut-directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome. https://pubmed.ncbi.nlm.nih.gov/27397586/







